When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
How to Get Used to CPAP
- For people who are new to CPAP therapy, getting used to the noise and physical sensation can take days, if not weeks.
- Many people struggle with wearing their CPAP mask at first. Tightening or loosening the mask can help ensure a more comfortable fit, but you can also ask your doctor about other mask types.
- A machine with a “ramp” feature, heated tubing, and a humidifier can also help you sleep comfortably and acclimate to CPAP therapy in a timely manner.
Continuous positive airway pressure (CPAP) can improve symptoms of obstructive sleep apnea (OSA) like snoring and daytime sleepiness , but it may take time to adjust to sleeping with the mask and other CPAP equipment .
To use a CPAP machine, you’ll wear a tight-fitting nasal mask over your nose or a full-face mask that covers both the nose and mouth. A machine pressurizes air to a specific level, then delivers the air through a hose that connects to the mask – this helps keep your breathing passages open while you sleep . It can take some time to get used to this sensation. Some people feel claustrophobic wearing the mask and experience side effects like dry mouth, congestion, and a runny nose.
You may find it hard to sleep during the first few nights of wearing a CPAP to bed. However, keeping your mask on for the whole night helps you acclimate faster and benefit from CPAP therapy . Below, learn how to get used to CPAP so you can sleep and breathe better every night.
Need a CPAP Prescription? Start Here.

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
How Long Does It Take to Get Used to CPAP?
Getting used to a CPAP takes about two weeks on average, but everyone responds on their own timeline. The first few nights and weeks may take some troubleshooting, and you should let your healthcare provider know if you have a hard time tolerating the therapy .
While scientific research hasn’t defined when most people get used to CPAP, studies have measured how many quit using it and when. In one study of 1,000 people, 54% stopped using their CPAP in the first month, and most of these respondents quit in the first two weeks . Another study of almost 2,000 people found that those who stuck with their CPAP for two months were much more likely to continue using it long term .
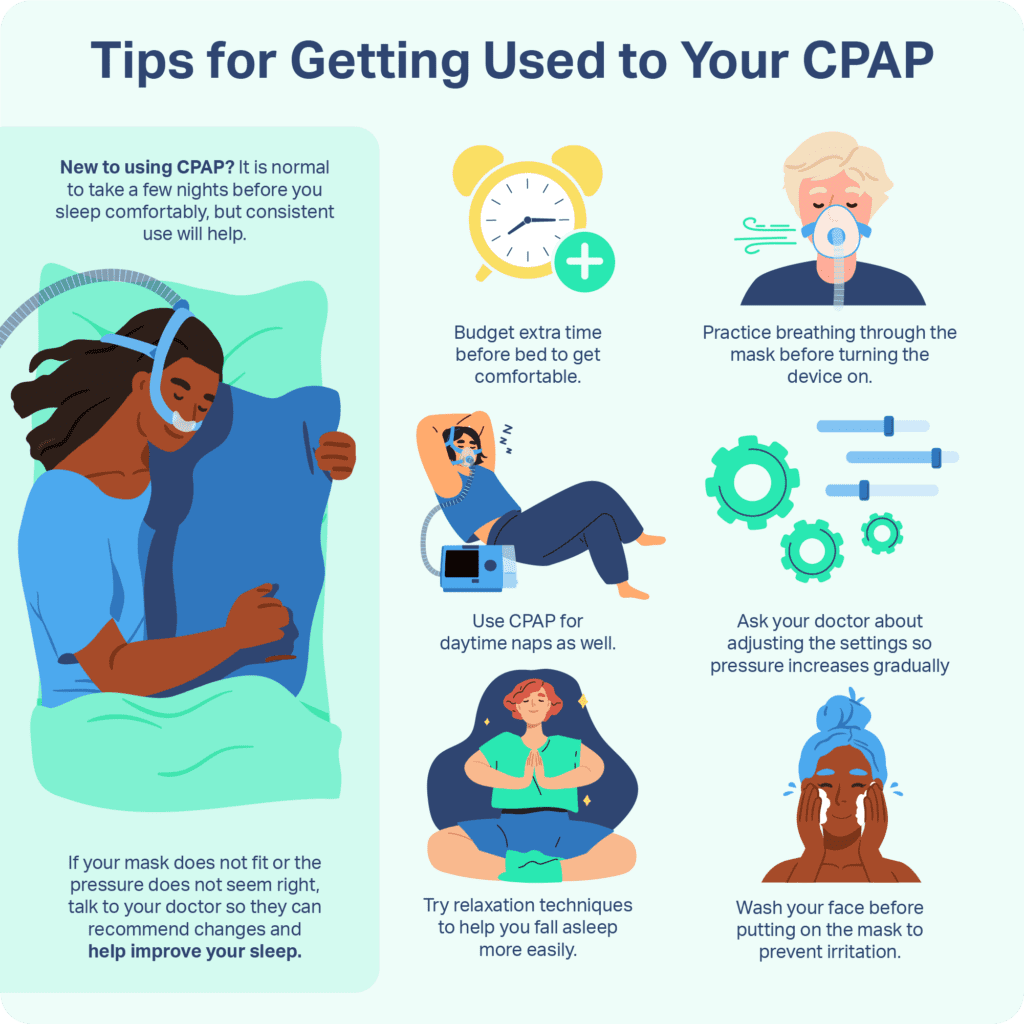
Tips for Getting Used to CPAP
Getting used to CPAP and continuing your therapy can help ensure effective sleep apnea treatment. The following tips can help you acclimate to CPAP more quickly.
Start Slow and Practice While Awake
To adjust to the sensation of airflow from your CPAP, you can try wearing the mask for short periods during the day, like when you’re watching TV. Each day, increase the amount of time you wear the CPAP mask until your body starts to adapt and recognize the sensation as normal.
Consider Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT), a type of therapy done by a mental health professional, challenges beliefs and patterns of thinking with the goal of changing behavior . CBT may help you get used to your CPAP. One study found that people who received CBT used their CPAP more hours per night than those who did not. For more information about this option, you can ask your provider to refer you to a specialist who performs CBT.
Use the Ramp Feature
You can ask your provider for a machine with an auto-ramp feature, which sets the air pressure at a lower setting when you begin your therapy. The pressure gradually increases to your prescribed level, helping you fall asleep more comfortably. Some ramp features are timed to increase pressure over a certain period, typically in the range of 30 to 60 minutes. Other devices have auto-ramp and will increase pressure only when the machine detects you’ve fallen asleep.
Make Sure Your Mask Fits Properly
Your CPAP mask is supposed to have a comfortable yet secure fit. If the mask feels too tight or doesn’t fit right, it can cause discomfort, air leaks, and even sores on your nose or cheeks. If your mask feels uncomfortable, your provider can help you adjust your straps, add cushioning, or even suggest a different mask type. You may also need a different mask type if you have facial hair because beards and mustaches can compromise the mask’s seal and cause air leaks .
Adjust Humidity and Temperature Settings
Adding humidified air to your CPAP can help with side effects like nasal dryness and make the experience more tolerable. Your provider can show you how to manage your CPAP humidifier and set the right moisture and temperature levels for optimal comfort.
Keep Equipment Clean
A dirty CPAP air filter or unsecure hose connection can make the machine noisier and make it harder to sleep. CPAP machines come with disposable filters or filters you can clean and reuse. You’ll find filter cleaning and replacement instructions in your manufacturer’s manual.
Cleaning and maintaining your connective hose, air filter, mask, and other CPAP equipment also helps prevent viruses and bacteria from building up and making you sick. Most supplies can be cleaned with mild soap and water, but check your manual for specific cleaning instructions .
Troubleshooting Common CPAP Issues
If you’re having a hard time getting used to your CPAP machine, you can address some of the common problems people have with their treatment to help ensure a faster adjustment period.
Claustrophobia
Pressurized air delivery from CPAP can make you uncomfortable, especially if you’re claustrophobic. If you can’t tolerate your mask, your provider can help you find a smaller or less intrusive mask. Some people also find that using nasal pillows – silicone or foam cushions positioned at both nostril openings – helps them feel less confined . A pressure ramp can also help decrease feelings of claustrophobia.
Difficulty Breathing
With pressurized air entering your airway during CPAP therapy, you may find it hard to exhale at first . If you can’t get used to this feeling, ask your provider about switching to an auto-titrating CPAP (APAP). These devices automatically decrease air pressure while you breathe out . Your provider may also recommend a BiPAP machine, which has different fixed pressure settings for inhaling and exhaling.
Dry Nose or Mouth
Waking up during the night or in the morning with a dry nose or mouth may tempt you to skip your CPAP altogether. Adding a heated connective hose or humidifier to your CPAP therapy can help you breathe comfortably throughout the night. Keep in mind these accessories often cost extra, and are not compatible with certain CPAP devices.
Stuffy Nose
CPAP therapy can cause your nasal passages to become red and swollen . Some people find that nasal saltwater sprays can help clear up a stuffy nose in the morning. If his symptom persists, ask your provider about relieving medications or trying another mask.
Skin Irritation
You don’t have to live with skin irritation and pressure sores from your CPAP mask. If your mask feels excessively uncomfortable or causes pain, you can ask your provider about loosening your straps or trying a different mask type . You can also try using mask liners to protect your skin and make wearing the mask more comfortable.
Mask Leaks
When you wear a nasal CPAP, air can sometimes leak out through your mouth . Air leaks around full-face masks typically happen because the mask doesn’t fit right or your humidifier or tubing has a faulty seal.
For mouth air leaks with a nasal CPAP, you can try adding a chin strap to keep your mouth closed or ask your provider about switching to a mask that covers both your mouth and nose. If your full-face mask is leaking air, your provider can readjust the straps, check your tubing, or recommend another mask. Some advanced CPAP systems include automatic leak detection with alerts when air pressure drops suddenly.
Noisy CPAP Machine
Most CPAP machines made today are fairly quiet. If the noise still keeps you from sleeping, you can try putting the machine under your bed to dampen any sounds as long as this doesn’t impede the hose connecting the device to your mask. If your CPAP machine is so loud you can’t sleep and you’re unable to get used to the noise, let your provider know – they can recommend a different machine or another treatment solution.
When to Talk to Your Doctor
CPAP therapy is the number one treatment for sleep apnea, but it only works if you wear it at least four hours a night, five to seven nights per week. If you have tried sleeping with your CPAP for a week and feel like it’s not getting any easier, let your provider know. They can work with you to tailor your mask, pressure settings, and humidification to find the most comfortable combination.
Frequently Asked Questions
What is the easiest CPAP mask to get used to?
Everyone has their own CPAP preferences, but many people say nasal pillow CPAP masks have fewer side effects and feel more comfortable than nasal or full-face masks. This mask type also has the best track record among users who stick with CPAP therapy in the long term .
What if I can’t fall asleep with my CPAP?
If you can’t fall asleep with your CPAP on, let your provider know. They may recommend trying a pressure ramp, wearing the mask for short periods at first until you adjust, or modifying the mask and machine settings. If you can use your CPAP all night, even through those first few rough nights, you will probably get used to it more quickly.
Can I skip a night of CPAP if I’m struggling to get used to it?
The best way to get used to a CPAP machine is to use it every night. If you skip a night, it may prolong your adjustment period.
Will I ever get comfortable sleeping with CPAP?
Most people eventually get comfortable using CPAP. It takes time and patience to get used to a CPAP, but you can choose from a wide range of options to find one that fits well and feels comfortable for sleep.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of product specialists, sleep health professionals, and people just like you. Whether you’re searching for the perfect mattress or need expert sleep advice, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
21 Sources
-
Dinh-Thi-Dieu, H., Vo-Thi-Kim, A., Tran-Van, H., & Duong-Quy, S. (2020). Efficacy and adherence of auto-CPAP therapy in patients with obstructive sleep apnea: a prospective study. Multidisciplinary respiratory medicine, 15(1), 468.
https://pubmed.ncbi.nlm.nih.gov/32153777/ -
NIH. CPAP – CPAP | NHLBI, NIH. www.nhlbi.nih.gov. Published 2022.
https://www.nhlbi.nih.gov/health/cpap -
Strohl, K. P. (2022, October). Sleep apnea. Merck Manual Consumer Version.
https://www.merckmanuals.com/home/lung-and-airway-disorders/sleep-apnea/sleep-apnea -
A.D.A.M. Medical Encyclopedia. (2023, April 20). Positive airway pressure treatment. MedlinePlus.
https://medlineplus.gov/ency/article/001916.htm -
Weaver, T. E. (2024, February 28). Assessing and managing nonadherence with continuous positive airway pressure (CPAP) for adults with obstructive sleep apnea. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/assessing-and-managing-nonadherence-with-continuous-positive-airway-pressure-cpap-for-adults-with-obstructive-sleep-apnea -
Patil, S. P., Ayappa, I. A., Caples, S. M., Kimoff, R. J., Patel, S. R., & Harrod, C. G. (2019). Treatment of adult obstructive sleep apnea with positive airway pressure: An American Academy of Sleep Medicine clinical practice guideline. Journal of Clinical Sleep Medicine, 15(2), 335–343.
https://pubmed.ncbi.nlm.nih.gov/30736887/ -
Dielesen, J., Ledwaba-Chapman, L. J., Kasetti, P., Husain, N. F., Skinner, T. C., Pengo, M. F., Whiteman, T., Asimakopoulou, K., Merritt, S., Jones, D., Dickel, P., Pulakal, S., Ward, N. R., Pepperell, J., Steier, J., & Sathyapala, S. A. (2025). Six early CPAP-usage behavioural patterns determine peak CPAP adherence and permit tailored intervention, in patients with obstructive sleep apnoea. Thorax, 80(5), 300–308.
https://pubmed.ncbi.nlm.nih.gov/40015971/ -
Jeppesen, K., Kørvel-Hanquist, A., Wolff, D. L., Petersen, S. R., Homøe, P., Kiær, E. K., Jennum, P. J., & Skjøt-Arkil, H. (2025). Patterns and stability of long-term adherence in continuous positive airway pressure therapy for obstructive sleep apnea: a cohort study. Sleep & breathing = Schlaf & Atmung, 29(4), 243.
https://pubmed.ncbi.nlm.nih.gov/40665080/ -
Weaver T. E. (2019). Novel Aspects of CPAP Treatment and Interventions to Improve CPAP Adherence. Journal of clinical medicine, 8(12), 2220.
https://pubmed.ncbi.nlm.nih.gov/31888148/ -
Blanco, M., Jaritos, V., Ernst, G., Salvado, A., Nogueira, F., & Borsini, E. (2018). Patients’ preferences and the efficacy of a hybrid model of a minimal contact nasal mask in patients with sleep apnea treated with CPAP. Sleep science (Sao Paulo, Brazil), 11(4), 254–259.
https://pubmed.ncbi.nlm.nih.gov/30746043/ -
Martinot, J. B., Hostaux, L., Malhotra, A., Hwang, D., & Pépin, J. L. (2024). Air leak phenotyping by mandibular jaw movement analysis in CPAP therapy: Key insights for practitioners. Respirology case reports, 12(9), e70030.
https://pubmed.ncbi.nlm.nih.gov/39319331/ -
Brown, L. & Lee, W. (2023 September). Titration of positive airway pressure therapy for adults with obstructive sleep apnea. In N. Collup & G. Finley (Ed.). UpToDate.
https://www.uptodate.com/contents/titration-of-positive-airway-pressure-therapy-for-adults-with-obstructive-sleep-apnea -
Nilius, G., Domanski, U., Schroeder, M., Woehrle, H., Graml, A., & Franke, K. J. (2018). Mask humidity during CPAP: influence of ambient temperature, heated humidification and heated tubing. Nature and science of sleep, 10, 135–142.
https://pubmed.ncbi.nlm.nih.gov/29750062/ -
Food and Drug Administration. (2024). Do You Need a Device That Claims to Clean a CPAP Machine?
https://www.fda.gov/consumers/consumer-updates/do-you-need-device-claims-clean-cpap-machine -
Rinaldo, V. (2022, March 2). Sleep-disordered breathing and CPAP. In Z. Mosenifar (Ed.). Medscape.
https://emedicine.medscape.com/article/870192 -
Patil, S. P., Ayappa, I. A., Caples, S. M., Kimoff, R. J., Patel, S. R., & Harrod, C. G. (2019). Treatment of adult obstructive sleep apnea with positive airway pressure: An American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. Journal of Clinical Sleep Medicine, 15(2), 301–334.
https://pubmed.ncbi.nlm.nih.gov/30736888/ -
Zhu, K., Aouf, S., Roisman, G., & Escourrou, P. (2016). Pressure-Relief Features of Fixed and Autotitrating Continuous Positive Airway Pressure May Impair Their Efficacy: Evaluation with a Respiratory Bench Model. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 12(3), 385–392.
https://pubmed.ncbi.nlm.nih.gov/26564383/ -
Koutsourelakis, I., Vagiakis, E., Perraki, E., Karatza, M., Magkou, C., Kopaka, M., Roussos, C., & Zakynthinos, S. (2011). Nasal inflammation in sleep apnoea patients using CPAP and effect of heated humidification. The European respiratory journal, 37(3), 587–594.
https://pubmed.ncbi.nlm.nih.gov/20595158/ -
Emami Zeydi A, Zare-Kaseb A, Nazari AM, Ghazanfari MJ, Sarmadi S. Mask-related pressure injury prevention associated with non-invasive ventilation: A systematic review. Int Wound J. 2024;21(6):e14909. doi:10.1111/iwj.14909
https://pubmed.ncbi.nlm.nih.gov/38826030/ -
Bachour A, Avellan-Hietanen H, Palotie T, Virkkula P. Practical Aspects of Interface Application in CPAP Treatment. Can Respir J. 2019;2019:7215258. Published 2019 Nov 3. doi:10.1155/2019/7215258
https://pubmed.ncbi.nlm.nih.gov/31781315/ -
Wimms, A., Ketheeswaran, S., Ziegenbein, C., Jennings, L., & Woehrle, H. (2016). Impact of a New Nasal Pillows Mask on Patients’ Acceptance, Compliance, and Willingness to Remain on CPAP Therapy. Sleep disorders, 2016, 6713236.
https://pubmed.ncbi.nlm.nih.gov/27648308/











































