At-Home Sleep Study
- What It Is: At-home sleep tests offer a convenient, affordable alternative to lab-based studies for diagnosing obstructive sleep apnea (OSA).
- How It Works: A home sleep study uses small sensors placed on your body to track your breathing patterns, oxygen levels, and heart rate overnight, with the data reviewed by a sleep specialist.
- What It Measures: A home sleep test typically measures airflow, breathing effort, blood oxygen levels, heart rate, and snoring to help detect signs of obstructive sleep apnea.
- Benefits and Limitations: Benefits of at-home testing include shorter wait times, lower cost, and the comfort of sleeping in your own bed. Limitations include under-detection of mild OSA and higher possibility of sensor errors.
Does snoring keep you or your partner up at night? Do you wake up repeatedly or wake up tired, with a dry mouth, sore throat, or headache? These are all possible signs of sleep apnea, a potentially serious sleep disorder that happens when your breathing is disrupted while you’re asleep.
Each year, many cases of obstructive sleep apnea (OSA) go undiagnosed. At-home sleep apnea testing is a convenient alternative to an in-lab sleep study. But at-home testing isn’t for everyone and may be most appropriate when sleep apnea is strongly suspected.
To see if a home sleep test (also known as an at-home sleep study) might be right for you, keep reading to find out more about what they are, how they work, and what they can—and can’t—do.
Don’t Just Test Your Sleep. Understand It.
Discover if sleep apnea is holding you back. You’ll get a personalized medical report and an expert consultation to help you take action.

What Is an At-Home Sleep Study?
A home sleep apnea test (HSAT or HST) involves a wearable device you use overnight, designed to help diagnose obstructive sleep apnea at home. As you sleep, the device monitors your breathing and oxygen levels to detect and measure pauses in breathing, which are known as apneas. The test calculates an OSA severity score by calculating the average number of lapses in breathing per hour in bed.
Types of Sleep Studies
Sleep tests are categorized by how much and what type of data they collect. Type 1 and 2 tests collect more detailed data and provide the most accurate diagnosis for OSA. Sleep lab or hospital-based polysomnography is a type 1 sleep test and is the better option for people who are suspected of having another medical condition or sleep disorder in addition to OSA .
Home sleep apnea tests are generally classed as type 3 or type 4. Type 3 tests use a greater number of sensors to capture relevant information such as blood oxygen levels, airflow, snoring, body position, or heart rate. However, type 3 tests don’t collect as much data as a type 1 or 2 test.
Home Sleep Test Equipment
The equipment you’ll receive for your home sleep test depends on the type of test your medical provider orders, and it may include all or some of the following in the list below.
- Nasal breathing sensor: These tubes are placed in your nostrils and wrapped behind your ears. They analyze breathing patterns by tracking air pressure from inhaling and exhaling.
- Effort belt: This is less common in home tests, but it’s a band that goes around your chest to measure movement associated with breathing. Data from this device can help differentiate between obstructive sleep apnea, where you’re making an effort to breathe, and central sleep apnea, where your brain doesn’t send the signal to inhale and exhale.
- Pulse oximeter: This device is usually placed over a fingertip to measure how much oxygen is in the blood.
- Microphone: Generally, the nasal breathing sensor estimates snoring, but sometimes an actual microphone is used to measure snoring. A sound sensor attached to the neck can also record sound and pressure.
- Data collection device: All of the sensors typically connect to the data collection device, either via wires or flexible tubes. This device may feature buttons you’re instructed to push when you want data collection to begin and end, as well as status lights to indicate the device is on and recording.
It’s important to note that most at-home tests don’t measure sleep quality. This may be limiting if you’re trying to decide whether an at-home test or onsite sleep study is better suited for your specific situation. Comparatively, polysomnography offers a more holistic overview of your sleep quality and sleep patterns in addition to the apnea-related metrics measured by at-home tests.
How Does an At-Home Sleep Study Work?
The process generally involves five steps: meeting with a medical professional, getting the equipment, doing the test, returning the equipment, then meeting again to discuss your results.
1. Schedule a visit with a care provider. A prescription is required to get a home sleep test, so if you’re experiencing symptoms of OSA, you’ll need to make an appointment with your provider. Many home sleep test companies offer virtual consultations for this purpose as well. If the provider thinks you could have sleep apnea, they will either prescribe you a home sleep test or refer you to a sleep specialist or sleep clinic.
2. Get your home sleep test. Once you have your prescription, depending on the device, it will either be mailed to you or you will need pick it up at a sleep lab or clinic. When you get the equipment, your provider will walk you through how to use it.
3. Take the test. Once you have the equipment, follow the instructions to put on any sensors required by the test. Try to go to sleep and wake up at your normal times and avoid caffeine and alcohol, as they can affect your sleep. If you usually take sleep medications, ask your doctor if it is appropriate to take them the night of the test.
4. Return your equipment. Unless you have a disposable test (like the WatchPAT One), bring or send the test back to the location predetermined by your provider. Once the clinic receives the equipment, they will download and analyze the collected data.
5. Review your results with your doctor. Once the data has been analyzed, your doctor or sleep specialist will discuss the results with you. They might give you a sleep apnea diagnosis and prescribe treatment such as a continuous positive airway pressure (CPAP) machine. Alternatively, they might inform you that your results were negative or inconclusive and ask that you undergo an in-lab sleep study.
What Does a Home Sleep Test Measure?
The metrics collected by a home sleep apnea test depend on the test type. To qualify as a type 3 test, a HSAT must measure:
- Two breathing-related measures, such as airflow and breathing effort
- Blood oxygen level
- One heart-related measure, like heart rate
Type 4 tests collect one or two measures, which may include:
- Airflow
- Blood oxygen level
- Heart rate
Other measurements, like snoring frequency, volume, and body movement, may also be collected.
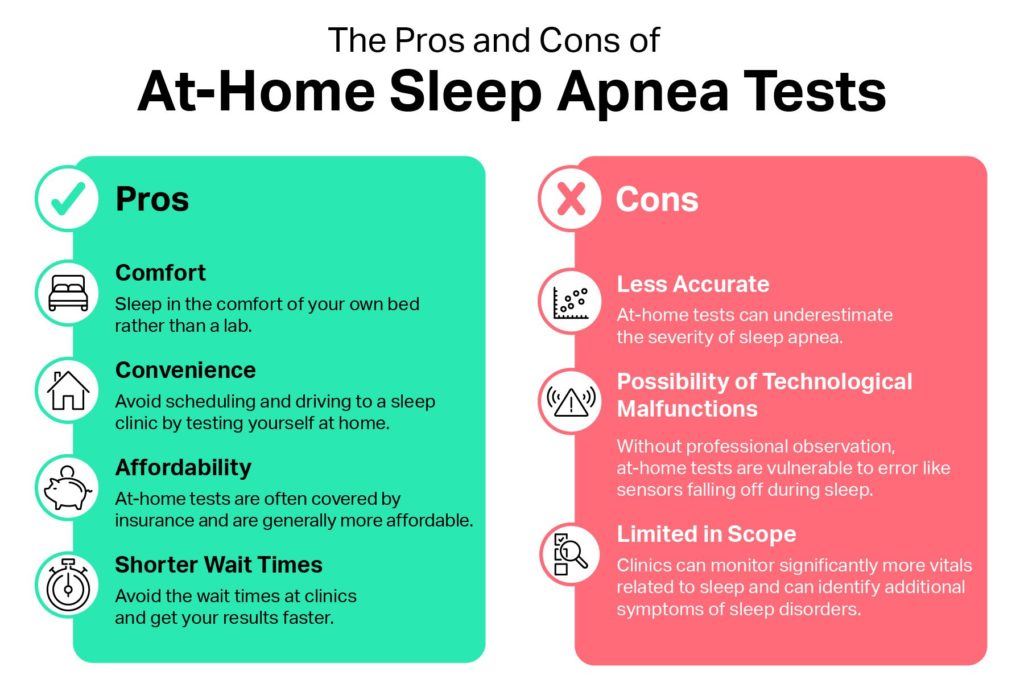
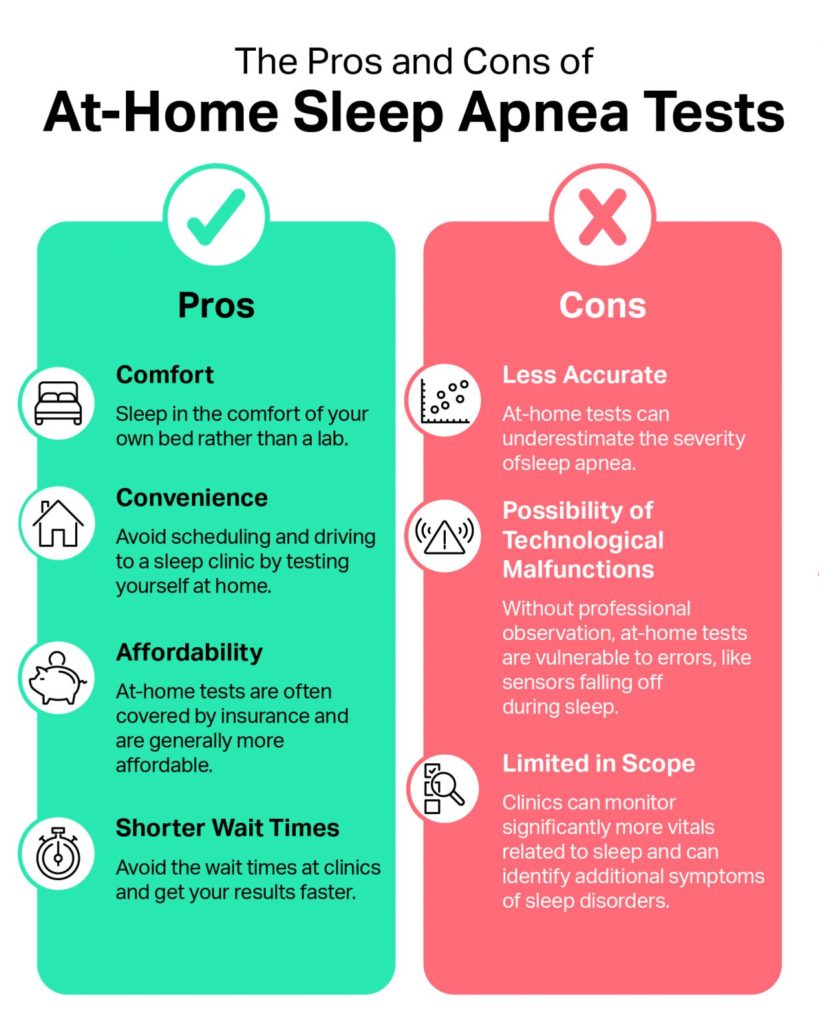
What Are the Benefits of an At-Home Sleep Test?
The key benefits of an at-home sleep apnea test compared to traditional polysomnography are shorter wait times and increased convenience, affordability, and comfort.
Comfort
The alternative to an at-home sleep apnea test is an overnight sleep study conducted in a lab. Sleep centers aim to make these comfortable by providing a nice bedroom. However, you’re still sleeping somewhere that feels unfamiliar, and there are technicians monitoring you while you sleep. A sleep apnea test at home may be preferable, as you can be in the comfort of your own home.
Convenience
At-home sleep apnea tests are generally more convenient than a polysomnogram. Instead of finding a sleep clinic, scheduling the overnight exam, and driving to and from the clinic, you can pick up the sleep apnea test at your local pharmacy or doctor’s office and administer the test yourself at home.
Affordability
At-home sleep apnea testing is generally more affordable than a polysomnogram and is often covered by insurance.
Shorter Wait Times
Whereas sleep clinics often have long waitlists, at-home sleep apnea tests can usually be administered more quickly as they don’t require you to come into the lab. The sooner you receive a diagnosis of OSA, the sooner you can start treatment and begin to find relief from your symptoms.
What Are the Limitations of an At-Home Sleep Test?
Taking a sleep apnea test at home offers many benefits, but there are some drawbacks to consider.
Less Accurate
When you take a sleep apnea test at home, the machine monitors your breathing once you turn it on. Instead of dividing the total number of respiratory events by your total sleep time, they are divided by the total amount of time you spend in bed, which tends to be longer.
As a result, at-home tests can underestimate the severity of sleep apnea by calculating an hourly rate that appears lower than it really is. By contrast, polysomnography is able to record when you’re sleeping and when you’re awake for a more accurate score.
Possibility of Technological Malfunctions
Since they aren’t overseen by a qualified health professional, home sleep tests are more vulnerable to errors. For example, it is possible for sensors to fall off or become dislodged while you’re sleeping, which you may not realize until you wake up. During a lab-based polysomnogram, on the other hand, a technician can reset the sensors and ensure everything is working as expected.
Limited in Scope
Home sleep apnea tests only monitor your breathing and oxygen levels. Overnight sleep studies monitor significantly more vitals related to sleep, including your brain waves and leg and eye movements. Because an at-home sleep apnea test doesn’t capture information about total sleep time, nighttime awakenings, or sleep stages, it cannot test for non-breathing-related sleep disorders, such as narcolepsy.
At-home sleep tests are generally only used to diagnose obstructive sleep apnea. They aren’t currently indicated for central sleep apnea, a rarer form of sleep apnea where the pauses in breathing are caused not by a collapse of the airways, but by the brain’s failure to send signals to breathe.
If the results of your at-home sleep test are inconclusive, or if you have additional symptoms that warrant a more comprehensive evaluation, your doctor may recommend an additional polysomnogram. It is also important to note that while an at-home sleep test can be used to diagnose obstructive sleep apnea, an overnight study in a sleep lab allows for therapeutic intervention such as CPAP therapy.
Which Type of Sleep Study Is Right for You?
Home sleep tests are only used to diagnose sleep-disordered breathing issues, like sleep apnea. In-lab sleep studies can help diagnose other sleep disorders, like narcolepsy and periodic limb movement disorders. The difference is in what the test measures. Though both usually measure airflow, blood oxygen levels, and heart rate, only in-lab sleep studies measure sleep by monitoring brain activity.
People often prefer a home sleep study to an in-lab study because they are less expensive and don’t require traveling to a sleep lab. A home test also involves fewer sensors attached to you as you sleep, so it may feel less invasive.
If you have a relatively straightforward case of suspected moderate or severe sleep apnea and no other health conditions, then a home sleep apnea test might be right for you. If you or your doctor have any reason to believe you need a more comprehensive test, then it might be worthwhile to skip the home test and go directly to the sleep lab, as results of a home sleep test may indicate further testing is needed.
Frequently Asked Questions
How much do home sleep studies cost?
In general, the cost of home sleep testing in the U.S. falls between $150 to $500. Often, health insurance covers some or all of the cost. You may need to pay the insurance deductible if you haven’t already.
Are at-home sleep studies accurate?
Type 3 home sleep apnea tests are highly accurate at detecting sleep apnea in people considered likely to have a moderate or severe form. The test becomes less accurate for people with mild cases of obstructive sleep apnea and may necessitate further testing in a clinical setting.
How many times can I take an at-home sleep apnea test?
Generally, people only take a home sleep apnea test once. If that test isn’t enough to diagnose obstructive sleep apnea, they may be advised to do an in-lab, overnight sleep study.
What sleep disorders can home tests detect?
Home sleep apnea testing is commonly used to detect sleep-disordered breathing problems, like obstructive sleep apnea. Since existing home tests rarely measure brain waves, they are typically not capable of diagnosing other sleep disorders.
Does insurance cover an at-home sleep study?
Many health insurance plans cover home sleep apnea tests. The amount of coverage depends on the insurance company and the medical provider. Medicare Part B, for example, requires people to pay fora portion of study costs as well as the deductible, if applicable. To be covered by insurance, a test generally needs to be prescribed by a sleep specialist. You may want to confirm that your specific test falls under your insurance coverage before taking it.
Who should not take a home sleep study?
Although a home sleep test is useful for many people who may have obstructive sleep apnea, a home sleep study may also be less accurate at detecting mild sleep apnea symptoms. Experts recommend an in-lab sleep study rather than a home study for people who are suspected to have congestive heart failure, severe or chronic pulmonary disease, or neurological or neuromuscular disorders. Individuals who are suspected to have other sleep disorders, like narcolepsy, parasomnias, or periodic limb movement disorder, should also consider an in-lab study.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
3 Sources
-
Kim, R. D., Kapur, V. K., Redline-Bruch, J., Rueschman, M., Auckley, D. H., Benca, R. M., Foldvary-Schafer, N. R., Iber, C., Zee, P. C., Rosen, C. L., Redline, S., & Ramsey, S. D. (2015). An economic evaluation of home versus laboratory-based diagnosis of obstructive sleep apnea. Sleep, 38(7), 1027–1037.
https://pubmed.ncbi.nlm.nih.gov/26118558/ -
Collop, N. A. (2010). Home sleep testing: It is not about the test. Chest, 138(2), 245–246.
https://pubmed.ncbi.nlm.nih.gov/20682524/ -
Sabil, A. K., Glos, M., Günther, A., Schöbel, C., Veauthier, C., Fietze, I., & Penzel, T. (2019). Comparison of apnea detection using oronasal thermal airflow sensor, nasal pressure transducer, respiratory inductance plethysmography and tracheal sound sensor. Journal of Clinical Sleep Medicine, 15(2), 285–292.
https://pubmed.ncbi.nlm.nih.gov/30736876/