When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
BiPAP vs. CPAP Machines
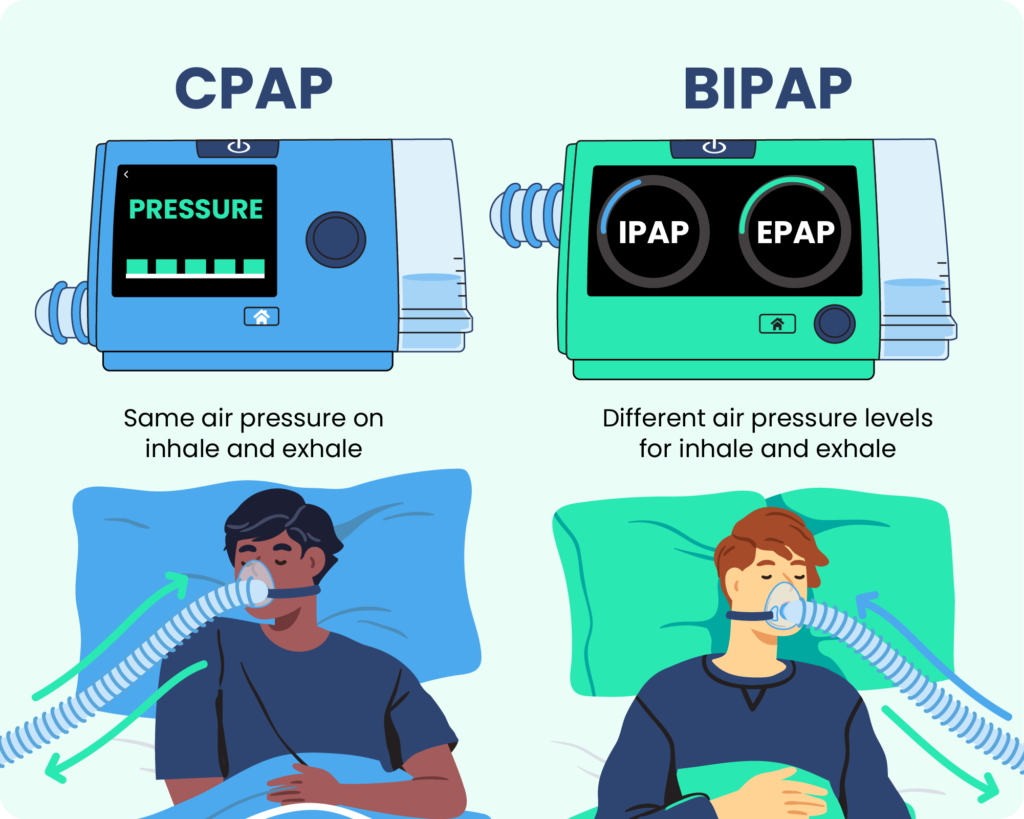
- CPAP provides constant air pressure, while BiPAP offers two pressure settings.
- BiPAP machines can automatically switch between an inhalation pressure and a lower exhalation pressure.
- A sleep specialist will recommend the right PAP therapy for you based on your sleep study results and individual needs.
Positive airway pressure (PAP) is one of the most common treatments for sleep apnea, a breathing disorder that affects approximately 10% to 30% of the population. The most common PAP treatment is continuous positive airway pressure (CPAP), but bilevel positive airway pressure (BiPAP or BPAP) may be a better option for some people.
While both forms of PAP therapy work in similar ways, their differences mean that each has distinctive benefits and drawbacks to consider. Because of this, the decision to switch PAP treatments should always be made under the advice of your health care team.

Exploring CPAP Machines — But Haven’t Been Tested Yet?
Start with our easy, at-home sleep test. It’s stress-free and effective. Get results within a few days.
What Is the Difference Between CPAP and BiPAP Machines?
CPAP and BiPAP machines are both forms of positive airway pressure therapy , which uses compressed air to open and support the upper airway during sleep. A portable machine generates the pressurized air and directs it to the user’s airway via a hose and mask system. Both systems use similar masks, hoses, and other accessories.
How Does CPAP Work?
In general, CPAP machines have an adjustable pressure setting that delivers between 4 to 20 cm H2O (a measure of air pressure that stands for centimeters of water pressure) regardless of whether the user is inhaling or exhaling. This pressure keeps air passages open and ensures the user can breathe properly, allowing them to avoid the pauses in breathing (or apneas) that are the primary symptom of sleep apnea.
The average setting is between 8 to 10 cm H2O . While CPAP machines have only one setting, some models now have a pressure relief option that allows for gentler air pressure on the exhale.
CPAP machines continuously pump air at one pressure setting rather than varying in pressure between the inhale and exhale, which can cause some people to feel as though they cannot exhale properly or that they are choking. Most users adjust to CPAP relatively quickly.
How Does BiPAP Work?
BiPAP machines have two pressure settings — inhalation positive airway pressure (IPAP) and exhalation positive airway pressure (EPAP) — that allow for lower pressure levels during exhalation.
Depending on the BiPAP machine’s settings, the switch between IPAP and EPAP may be timed or automatically based on the user’s breathing patterns. BiPAP machines have a typical pressure range of 4 to 30 cm H2O. Both BiPAP and CPAP settings must be determined in an overnight sleep study, or polysomnography.
BiPAP machines have up to three settings for the switch between IPAP and EPAP.
- Spontaneous: Spontaneous switching automatically senses the user’s breathing pattern and switches between the two pressure levels when they naturally inhale and exhale. The majority of BiPAP users rely on this setting, and it is standard for BiPAP devices.
- Timed: Timed switching allows users to program how long each IPAP and EPAP phase should last. This ensures users take the correct number of breaths per minute and can function much like a ventilator.
- Spontaneous/timed: This setting is primarily spontaneous, following the user’s natural breathing patterns. On this setting, timed switching turns on when the machine senses that the user has dropped below a set number of breaths per minute.
Additionally, BiPAP machines can be fixed or auto-adjusting.
- Fixed: The IPAP and EPAP settings of a fixed BiPAP machine are pre-set and do not change throughout the night.
- Auto-adjusting: An auto-adjusting BiPAP machine has a range set for both IPAP and EPAP. This allows the machine to adjust automatically throughout the night in response to how the sleeper is breathing.
CPAP vs. BiPAP
Different types of PAP therapy work better for different conditions, though there is some overlap . CPAP therapy is generally recommended for obstructive sleep apnea (OSA), and sleep specialists are unlikely to place someone with OSA on BiPAP unless they cannot tolerate CPAP treatment.
While some insurance providers cover both CPAP and BiPAP for OSA, those that do usually require proof that CPAP treatment is inadequate or not tolerated before reimbursing for a BiPAP machine. BiPAP therapy is primarily used to treat central sleep apnea (CSA), as well as heart, lung, and neurological disorders that require structured airway support during sleep.
Unlike BiPAP machines, CPAP machines are available in a range of sizes. The most common type is intended to be used at home and is slightly smaller than a shoebox, while travel versions may be small enough to fit in the palm of your hand. Travel models sometimes have backup batteries for use while camping, and FAA-approved models are available for use on planes.
Both CPAP and BiPAP machines are available with a range of accessories, both integrated and after-market. The most common are data collection features and climate control features like humidifiers and heated tubing.
| CPAP | BiPAP | |
|---|---|---|
| Typical Cost | $500-$1000 | $1,700-$3,000 |
| Pressure Levels | 1 | 2 |
| Typical Pressure Range | 4 to 20 cm H2O | 4 to 30 cm H2O |
| Insurance Coverage | May be covered | May be covered if CPAP therapy fails or is contraindicated |
BiPAP vs. CPAP: Which Is Best for You?
Although CPAP and BiPAP machines may seem similar, their differences can have a significant impact on your treatment. Because of this, the decision to switch from one to another should always be made with your health care team.
CPAP users usually have an adjustment period before they feel comfortable using their machines. Discomfort can be managed by adjusting settings, experimenting with climate control accessories or different mask types, or using a machine that slightly reduces air pressure on the exhale. BiPAP treatment is available for patients who do not tolerate CPAP therapy, but this switch must be decided on and supervised by a sleep specialist.
Who Is CPAP Best For?
CPAP therapy is often the first-line treatment for obstructive sleep apnea and works well for many people, especially those who:
- Have moderate to severe obstructive sleep apnea
- Need a consistent, fixed pressure to keep the airway open
- Tolerate steady airflow without difficulty exhaling
- Want a widely covered and well-studied treatment option
- Prefer a simpler device without automatic pressure changes
Who Is BiPAP Best For?
BiPAP therapy delivers different pressures for inhalation and exhalation and may be recommended for people who:
- Have trouble exhaling against CPAP pressure
- Require higher pressure settings to treat sleep apnea
- Experience aerophagia (air swallowing) or discomfort on CPAP
- Have complex sleep apnea, central sleep apnea, or certain lung or neuromuscular conditions
- Need more advanced pressure support based on medical guidance
Frequently Asked Questions
Is a BiPAP machine bigger than a CPAP?
BiPAP machines are generally similar in size to CPAP machines, though some models may be slightly larger due to additional pressure settings and features. In most cases, the difference is minimal, and both types are designed to fit easily on a nightstand or travel with you when needed.
Is a pressure ramp feature available on a BiPAP machine?
Yes. Many BiPAP machines include a ramp feature, which starts therapy at a lower pressure and gradually increases it over time. This can make it easier to fall asleep, especially for people who are sensitive to higher pressures.
How do you know if BiPAP is working?
BiPAP therapy is likely working if you experience improved sleep quality, fewer nighttime awakenings, reduced daytime sleepiness, and relief from symptoms like shortness of breath or morning headaches. Your machine’s therapy data—such as usage, leak rates, and breathing events—can also help your provider determine whether treatment is effective. If symptoms persist, a follow-up visit may be needed to adjust settings.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of product specialists, sleep health professionals, and people just like you. Whether you’re searching for the perfect mattress or need expert sleep advice, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
6 Sources
-
Kline, L. R. (2022, April 1). Clinical presentation and diagnosis of obstructive sleep apnea in adults. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-obstructive-sleep-apnea-in-adults -
Pinto V.L., & Sharma S. (2022, May 2). Continuous positive airway pressure. In StatPearls. StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK482178/ -
Brown, L. K. & Lee, W. (2021, September 17). Titration of positive airway pressure therapy for adults with obstructive sleep apnea. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/titration-of-positive-airway-pressure-therapy-for-adults-with-obstructive-sleep-apnea -
National Heart, Lung, and Blood Institute. (2022, March 24). CPAP.
https://www.nhlbi.nih.gov/health/cpap -
Farré, R., Gozal, D., & Montserrat, J. M. (2021). Alternative procedure to individual nasal pressure titration for sleep apnea. Journal of Clinical Medicine, 10(7), 1453.
https://pubmed.ncbi.nlm.nih.gov/33916282/ -
Antonescu-Turcu, A., & Parthasarathy, S. (2010). CPAP and bi-level PAP therapy: New and established roles. Respiratory Care, 55(9), 1216–1229.
https://pubmed.ncbi.nlm.nih.gov/20800002/














































