When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Snoring: Harmless or Dangerous?
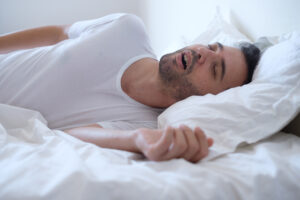
Snoring occurs when airflow is blocked or restricted in the nasopharynx, an area of the upper airway located behind your nose, causing tissues in the airway to flutter and produce sound. While snoring on its own is usually considered a harmless – albeit highly disruptive – phenomenon, for some people it indicates a more serious underlying medical condition or sleep disorder.
Is Snoring Dangerous?
Generally, infrequent snoring is normal and typically not a cause for concern. However, the severity of snoring can range from light and barely audible to heavy and disruptive. Primary snoring can be more disruptive, but is not usually seen as a health concern unless there are signs of breathing problems or sleep apnea.
For some people, heavy snoring indicates the presence of sleep apnea, a sleep-related breathing disorder that causes people to choke or gasp for air in their sleep.
Is Your Snoring a Health Risk?
Answer three questions to understand if you should be concerned.
Causes of Snoring
While snoring does not necessarily indicate the presence of a sleep disorder, it can disrupt sleep for you and your partner. Snoring is associated with obesity and old age even for those who do not have sleep apnea symptoms. Other risk factors for snoring include:
- Weight gain
- Enlarged tonsils or adenoids
- Endocrine disorders
- Genetic syndromes
- Consumption of sedatives or alcohol
- Chronic nasal congestion or blockage
- A relatively small or displaced jaw
- Pregnancy
- Postmenopausal status
Another common cause of snoring is back sleeping, which can affect breathing by restricting the airway. People who snore are often encouraged to sleep on their sides instead.
Should I See a Doctor About Snoring?
Snoring is considered the chief symptom of obstructive sleep apnea (OSA), a condition attributed to a physical blockage that restricts respiratory activity in the upper airway. Roughly 2-9% of adults live with OSA. Episodes involving a complete loss of airflow are called apneas, and episodes with reduced airflow are known as hypopneas.
| Adult AHI | Pediatric AHI | |
|---|---|---|
| Mild OSA | ≥ 5 to < 15 events per hour | ≥ 1 to ≤ 5 events per hour |
| Moderate OSA | ≥ 15 to < 30 events per hour | > 5 to ≤ 10 events per hour |
| Severe OSA | ≥ 30 events per hour | > 10 events per hour |
Considering each apnea normally lasts at least 30 seconds, even mild OSA can be disruptive to the sleeper and anyone who shares their bed. Snoring may accompany apnea-hypopnea episodes or occur independently during the night. Excessive daytime sleepiness from not getting enough rest is another common symptom of OSA.
Central sleep apnea, which occurs when the brain cannot properly signal the muscles that control breathing, may also produce snoring, but this is less common. Another sleep disorder, upper airway resistance syndrome, can cause snoring due to airway restriction but does not include apnea or hypopnea episodes. Additionally, sleep-related bruxism – also known as nocturnal teeth-grinding – is associated with snoring, particularly in children.
Any sleep disorder should be taken seriously. If you or your partner are concerned about heavy snoring, you should schedule a visit with your doctor to discuss the situation. People with OSA often benefit from continuous positive air pressure (CPAP) therapy, which administers air that is pressurized at a prescribed rate to ease breathing during the night.
How to Stop Snoring
If you ask your doctor about snoring, they may recommend an examination of the nose and mouth to check for a physical obstruction, as well as other warning signs such as nasal polyps, a high or narrow arched palate, a displaced jaw, or enlarged tonsils or adenoids.
You may be able to reduce your snoring by simply making certain lifestyle changes. These include losing weight, avoiding alcohol and sedative medications at night, and always sleeping on your side. Since nasal congestion can cause breathing, treating this with decongestants or corticosteroid sprays may be effective if your doctor approves them.
Anti-snoring mouthguards have proven effective for some people. Tongue-retaining devices (TRDs) form a seal around the tongue and hold it in place. These appliances can alleviate snoring for people whose tongues tend to fall in the back of their throat when they sleep. Mandibular advancement devices (MADs) physically move the tongue and jaw forward, allowing for maximum airflow.
In certain cases, surgery may be advised. During a uvulopalatopharyngoplasty procedure, the patient’s uvula, palate, and pharyngeal walls are removed to create more space for the upper airway. However, this is a procedure that requires general anesthesia and may not be the most practical – or cost-effective – way to correct snoring.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
3 Sources
-
NIH Office of Communications and Public Liaison. (2017, July). Struggling to Sleep? Don’t Let Apnea Steal Your Sweet Dreams. NIH News in Health.
https://newsinhealth.nih.gov/2017/07/struggling-sleep -
Strohl, Kingman P. (2020, Sept). Obstructive Sleep Apnea. Merck Manual Professional Version.
https://www.msdmanuals.com/professional/pulmonary-disorders/sleep-apnea/obstructive-sleep-apnea -
MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); Snoring;
https://medlineplus.gov/snoring.html