When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
CPAP Machine Side Effects
- CPAP therapy can cause a range of side effects, including aerophagia (air swallowing), skin irritation, claustrophobia, nasal congestion, dry nose or mouth, and upper respiratory infections.
- Mask discomfort and poor fit are common contributors to side effects, such as pressure marks, dermatitis, or dryness around the nose and mouth.
- Many side effects can be minimized with adjustments like trying a different mask type, adding heated humidification, or working with a sleep specialist to optimize pressure settings.
CPAP machines can reduce the symptoms of sleep apnea and improve quality of life for people living with this condition. Despite the effectiveness of CPAP therapy as a treatment for sleep apnea, some people choose not to use their device consistently because of unwanted side effects .
For people new to CPAP or those struggling to use their CPAP machine consistently, we cover information about common CPAP side effects and strategies to improve the comfort of CPAP therapy.

Exploring CPAP Machines — But Haven’t Been Tested Yet?
Start with our easy, at-home sleep test. It’s stress-free and effective. Get results within a few days.
Common CPAP Side Effects
While CPAP therapy is highly effective for treating sleep apnea, it can take time for the body to adjust to wearing a mask and breathing pressurized air each night. During this adjustment period, some people experience side effects that range from mild discomfort to sleep disruption.
Understanding the most common CPAP side effects can help you recognize what’s normal, identify potential problems early, and know when simple adjustments—or medical guidance—may be needed.
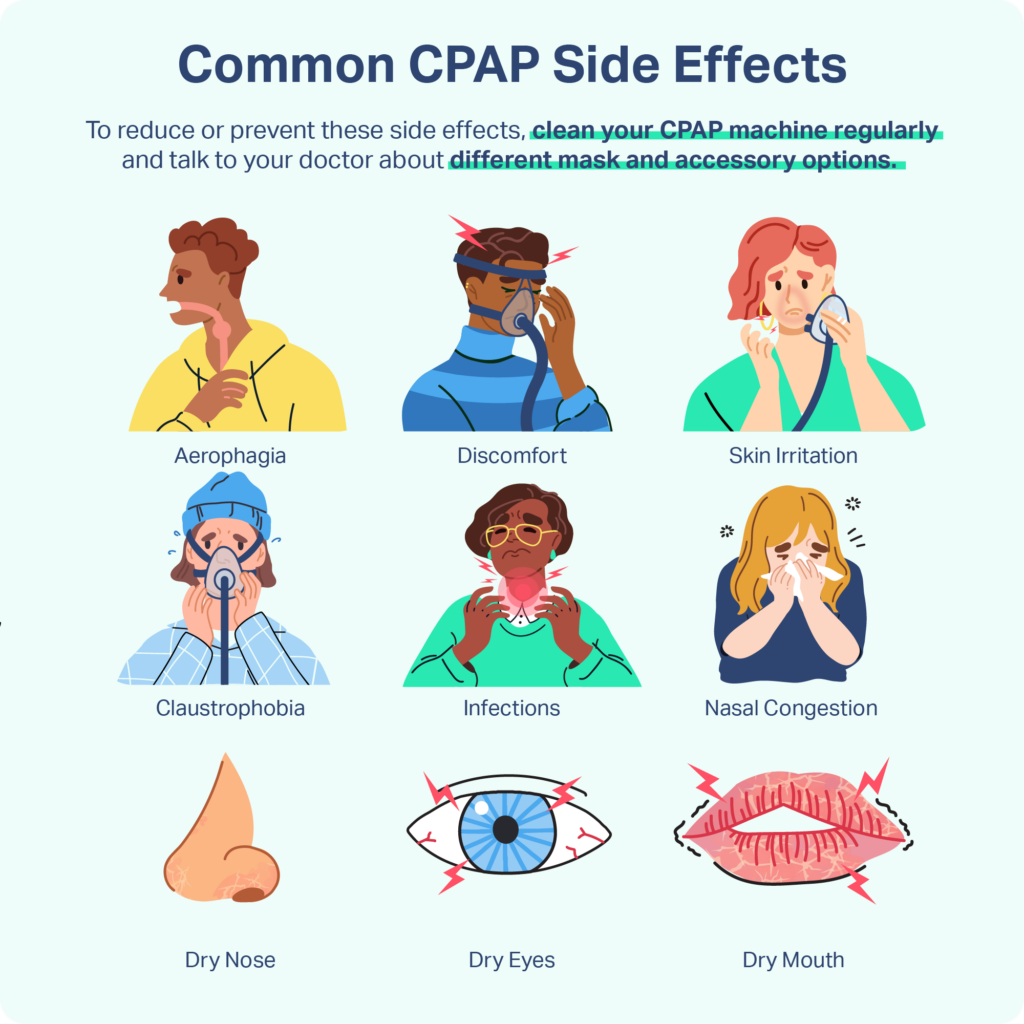
Aerophagia
Aerophagia happens when a person swallows too much air . A person with aerophagia may experience abdominal discomfort, flatulence, and belching because of the buildup of air in the gastrointestinal system. About 16% of CPAP users experience aerophagia due to swallowing pressurized air from the CPAP machine.
To reduce aerophagia , some CPAP users may benefit from switching to an automatic positive airway pressure (APAP) machine. While CPAP continuously uses the same level of air pressure, APAP alternates air pressure levels based on the sleeper’s breathing and snoring.
Skin Irritation
For some CPAP users, the CPAP mask can cause discomfort. Improperly fitting masks can create rashes and pressure sores on the cheeks or nose. CPAP users sometimes report that mask use interferes with a hairstyle or leaves unwanted imprints on the face.
CPAP masks can also contribute to dermatitis, a condition in which the skin becomes inflamed after coming into contact with certain substances. People who have dry skin prior to using CPAP have a greater likelihood of developing dermatitis.
Materials in the mask, such as silicone, can cause a reaction called allergic dermatitis. Common side effects of allergic dermatitis include redness and itching. In extreme cases, people with allergic dermatitis may experience blistering on the skin.
Claustrophobia
The fear of closed-in spaces, or claustrophobia, is a commonly reported side effect of CPAP . Many CPAP users feel confined while wearing a mask that covers the nose. Researchers estimate that more than half of CPAP users with obstructive sleep apnea have claustrophobic tendencies when starting to use the device.
CPAP users who continue to experience claustrophobia may prefer nasal pillows that are inserted into the nostrils, rather than using a nasal mask that covers the nose or a full-face mask that covers the nose and mouth. Another strategy is to wear the mask for short periods during restful activities, such as reading. This daytime wear can increase tolerance of both the mask and the CPAP pressure, making it more comfortable to use at night.
Respiratory Infections
People who use CPAP machines may develop upper respiratory infections or sinus infections. Bacteria and viruses in the mouth, throat, and lungs can enter the CPAP mask or hose while a person breathes during sleep. Allergens such as mold and dust can also enter the mask or hose.
If a CPAP machine isn’t cleaned properly, germs and allergens can build up within the device and may lead to illness.
Nasal Congestion and Dry Nose
Nasal congestion and runny nose can occur with CPAP use. People undergoing CPAP therapy may also experience dry nose from the forced air flowing into the nose. The flow of dry air can lead to nosebleeds and crusting. Dry noses with CPAP use are particularly common in climates with cold weather or low humidity.
Dry Mouth and Eyes
People who use CPAP machines may experience dry mouth or dry eyes as a result of mask leaks. Mask leaks can occur when air enters through the nose and exits through the mouth. CPAP users who cannot close their mouths against the equipment or who breathe through their mouths while sleeping may experience dry mouth.
Mask leaks may also happen when a mask doesn’t fit properly or doesn’t seal well. Masks that don’t provide an adequate seal may allow pressurized air to flow from the top of the mask toward the eyes. CPAP mask leaks can lead to dry eyes, which may be irritating and uncomfortable for the CPAP user.
Tips for Preventing CPAP Side Effects
Side effects of CPAP may discourage people from using their devices. By reducing or preventing side effects, CPAP users are more likely to use their devices consistently and experience the benefits of CPAP therapy.
Choose the Right Face Mask
Choosing a CPAP face mask that is comfortable and seals well can help reduce or prevent the side effects of CPAP therapy. Face masks come in a variety of styles and sizes. Nasal masks cover only the nose, while full-face masks cover both the nose and mouth. Nasal pillows are less obtrusive and cover just the nostrils, though they typically aren’t suitable for people who require high CPAP pressure settings.
CPAP users may need to try several styles and sizes before determining which mask is most comfortable and seals well. Ultimately, the best mask is the one that leads to consistent use of the CPAP machine.
In some cases, people may develop CPAP side effects after using their machine for a period of time because of weight or dental changes. Adding cushioning, selecting a new style of mask, or resizing a current mask may help resolve side effects.
Clean CPAP Machines Regularly
The CPAP mask and tubing should be cleaned daily because germs, mold, and dust can become trapped in the device. The Food and Drug Administration recommends following the device manufacturer’s instructions for cleaning. Face masks and hoses can typically be cleaned with gentle soap and warm water.
Devices are available that claim to disinfect CPAP equipment with ozone gas or ultraviolet light. However, the FDA has cautioned consumers that it hasn’t yet determined whether these devices are safe or effective.
Consider CPAP Accessories
CPAP users who experience unwanted side effects may find relief with CPAP accessories or supplies.
- Chin strap: A chin strap helps keep a person’s mouth closed during sleep. Chin straps can help prevent air leaks and reduce aerophagia symptoms that result from swallowing air.
- Humidifiers: Some CPAP users experience dry mouth or dry nasal passages from inhaling pressurized air. Using a CPAP humidifier to add moisture to the pressurized air or humidifying the bedroom with a room humidifier can help alleviate dryness. Some CPAP humidifiers include a heating element to warm the air that is delivered through the hose and mask.
- Heated tubes: Humid airflow can create excess condensation in a CPAP tube or even cause water to drip onto the user’s face. Heated tubes can prevent this unwanted condensation.
- Mask liners: Mask liners provide an extra layer between the face and mask. The use of mask liners can reduce facial discomfort or skin irritation.
- Barrier creams: Using barrier creams or gels can reduce skin irritation while wearing a CPAP mask.
- Moisturizers: Petroleum-free moisturizers can reduce discomfort caused by a CPAP mask and relieve dry or irritated skin.
- Nasal sprays: CPAP users with stuffy noses may find saltwater nasal sprays helpful in relieving congestion.
Adjusting CPAP Pressure to Avoid CPAP Side Effects
Typically, the appropriate CPAP pressure for an individual is determined during an overnight sleep study. However, in the first weeks of CPAP use, pressure levels may need to be adjusted to reduce the risk of side effects.
Additionally, if the CPAP user’s lifestyle or body changes, the CPAP pressure may need to be adjusted. Changes that may affect the appropriate pressure include fluctuations in weight and the use of sedatives or alcohol.
Some CPAP users may benefit from using a pressure ramp. Rather than initiating the full CPAP pressure at once, a pressure ramp is a feature on some CPAP machines that increases pressure over a specific period of time set by a health care provider. A pressure ramp allows the CPAP user to fall asleep before feeling the full pressure from the machine.
When to Talk to a Doctor
If you experience uncomfortable side effects when using your CPAP machine at any point in your treatment, consult your doctor.
People who use CPAP machines typically meet with a health care provider one to eight weeks after starting treatment. During this follow-up visit, your doctor will ask about your symptoms and may review data from your device. Your provider can make adjustments to your CPAP machine based on your needs and can offer other treatment suggestions if appropriate.
Medical Disclaimer: The content on this page should not be taken as medical advice or used as a recommendation for any specific treatment or medication. Always consult your doctor before taking a new medication or changing your current treatment.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of product specialists, sleep health professionals, and people just like you. Whether you’re searching for the perfect mattress or need expert sleep advice, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
17 Sources
-
National Heart, Lung, and Blood Institute. (2022, March 24). CPAP.
https://www.nhlbi.nih.gov/health/cpap -
Weaver, T. E. (2021, September 28). Assessing and managing nonadherence with continuous positive airway pressure (CPAP) for adults with obstructive sleep apnea. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/assessing-and-managing-nonadherence-with-continuous-positive-airway-pressure-cpap-for-adults-with-obstructive-sleep-apnea -
Abraczinskas, D. (2021, January 5). Overview of intestinal gas and bloating. In N. J. Talley (Ed.). UpToDate.
https://www.uptodate.com/contents/overview-of-intestinal-gas-and-bloating -
Shirlaw, T., Hanssen, K., Duce, B., & Hukins, C. (2017). A randomized crossover trial comparing autotitrating and continuous positive airway pressure in subjects with symptoms of aerophagia: Effects on compliance and subjective symptoms. Journal of Clinical Sleep Medicine, 13(7), 881–888.
https://pubmed.ncbi.nlm.nih.gov/28558864/ -
Brown, L. K. & Lee, W. (2021, September 17). Titration of positive airway pressure therapy for adults with obstructive sleep apnea. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/titration-of-positive-airway-pressure-therapy-for-adults-with-obstructive-sleep-apnea -
Kryger, M. H., & Malhotra, A. (2022, May 23). Management of obstructive sleep apnea in adults. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/obstructive-sleep-apnea-overview-of-management-in-adults -
Ghadiri, M., & Grunstein, R. R. (2020). Clinical side effects of continuous positive airway pressure in patients with obstructive sleep apnoea. Respirology, 25(6), 593–602.
https://pubmed.ncbi.nlm.nih.gov/32212210/ -
Soundararajan, V., Lor, J., & Fishbein, A. B. (2020). Sleep apnea and skin. Current Sleep Medicine Reports, 6(3), 94–100.
https://pubmed.ncbi.nlm.nih.gov/33767945/ -
A.D.A.M. Medical Encyclopedia. (2021, August 14). Contact dermatitis. MedlinePlus.
https://medlineplus.gov/ency/article/000869.htm -
MedlinePlus: National Library of Medicine (US). (2016, August 9). Phobias.
https://medlineplus.gov/phobias.html -
Rinaldo, V. (2022, March 2). Sleep-disordered breathing and CPAP. In Z. Mosenifar (Ed.). Medscape.
https://emedicine.medscape.com/article/870192 -
Edmonds, J. C., Yang, H., King, T. S., Sawyer, D. A., Rizzo, A., & Sawyer, A. M. (2015). Claustrophobic tendencies and continuous positive airway pressure therapy non-adherence in adults with obstructive sleep apnea. Heart & Lung, 44(2), 100–106.
https://pubmed.ncbi.nlm.nih.gov/25744632/ -
A.D.A.M. Medical Encyclopedia. (2020, January 29). Positive airway pressure treatment.
https://medlineplus.gov/ency/article/001916.htm -
Patil, S. P., Ayappa, I. A., Caples, S. M., Kimoff, R. J., Patel, S. R., & Harrod, C. G. (2019). Treatment of adult obstructive sleep apnea with positive airway pressure: An American Academy of Sleep Medicine clinical practice guideline. Journal of Clinical Sleep Medicine, 15(2), 335–343.
https://pubmed.ncbi.nlm.nih.gov/30736887/ -
U.S. Food and Drug Administration. (2020, February 27). CPAP machine cleaning: Ozone, UV light products are not FDA approved.
https://www.fda.gov/consumers/consumer-updates/cpap-machine-cleaning-ozone-uv-light-products-are-not-fda-approved -
Genta, P. R., Kaminska, M., Edwards, B. A., Ebben, M. R., Krieger, A. C., Tamisier, R., Ye, L., Weaver, T. E., Vanderveken, O. M., Lorenzi-Filho, G., DeYoung, P., Hevener, W., & Strollo, P. (2020). The importance of mask selection on continuous positive airway pressure outcomes for obstructive sleep apnea. An official American Thoracic Society workshop report. Annals of the American Thoracic Society, 17(10), 1177–1185.
https://pubmed.ncbi.nlm.nih.gov/33000960/ -
Freedman, N. & Kuzniar, T. J. (2021, March 4). Mode selection for titration of positive airway pressure in adults with obstructive sleep apnea. In S. M. Harding (Ed.). UpToDate.
https://www.uptodate.com/contents/mode-selection-for-titration-of-positive-airway-pressure-in-adults-with-obstructive-sleep-apnea