When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
CPAP Pressure Settings
- CPAP pressure levels are typically the lowest amount of pressure needed to to keep the airway open.
- Most CPAP machines operate within a pressure range of 4 to 20 cm H2O, and the average setting for people with sleep apnea tends to be around 9 cm H2O.
- If your CPAP pressure is too low, you may experience symptoms like snoring, daytime sleepiness, or continued apnea events. If it’s too high, you may experience discomfort while exhaling, dry mouth, or aerophagia.
- Talk to your doctor about adjusting your CPAP pressure if you experience discomfort, breathing difficulties, or a lack of symptom improvement.
CPAP pressure settings determine how much air your machine delivers to keep your airway open while you sleep. And getting them at the correct level is essential for comfortable, effective sleep apnea treatment. People with obstructive sleep apnea (OSA) stop breathing for brief intervals during sleep due to a blocked or collapsed airway, but CPAP machines deliver pressurized air to help normalize breathing.
Below, we’ll discuss how CPAP pressure is measured, the various factors that determine pressure needs, and the signs and symptoms that suggest your pressure level might need adjusting. It’s important to contact your doctor if you believe your CPAP machine settings need to be adjusted. Pressure settings should only be changed under the guidance of a medical professional.
How CPAP Pressure Settings Are Determined
Pressure in a CPAP machine is measured in centimeters of water pressure (cm H2O). Settings vary based on the device, but most CPAP machines have a pressure range of 4 cm H2O to 20 cm H2O. The average pressure setting for people with OSA is around 9 cm H2O .
CPAP Titration Study
A CPAP titration study is the most common method used to determine an appropriate pressure level. Similar to a sleep study, the assessment is usually done overnight at a sleep center or hospital. Sensors are attached to the sleeper’s body to monitor oxygen levels, breathing, heart rate, brain waves, and body movements. A physician or sleep specialist calibrates CPAP pressure levels until the lowest amount of pressure needed to keep the airway open is determined.
The apnea-hypopnea index (AHI) assesses how many times a person stops breathing or breathes shallowly while asleep, which helps medical professionals determine CPAP pressure settings. Most modern CPAP machines keep track of the sleeper’s AHI, which lets the doctor know if the pressure level needs to be modified.
The sleeper is also fitted for a CPAP mask during the study, which is crucial for effective treatment. CPAP masks come in a variety of styles, including full-face masks, nasal masks, and nasal pillows.After the study, the doctor establishes the optimal pressure range. They can also make recommendations about how to use a CPAP machine.
APAP Machine
Your doctor might also prescribe an auto-adjusting positive airway pressure (APAP) machine. This device automatically changes pressure levels based on a user’s breathing patterns. The machine starts at a low setting and then increases according to changes in breathing and airway resistance.
Even though APAP machines automatically adjust pressure levels, a physician still needs to prescribe an ideal pressure range suited to your needs. If the range is off, you may experience adverse side effects.
What Should My CPAP Pressure Be?
A physician determines proper pressure settings based on your CPAP titration study and AHI. Your pressure might need to be adjusted later if you lose or gain significant weight, change your sleep position, or start taking certain medications. Always speak with your doctor if you suspect your pressure level needs fine-tuning.
Factors That Affect CPAP Pressure Settings
A number of factors determine the severity of OSA and a person’s appropriate CPAP pressure setting. Some are anatomical, while others relate to lifestyle and sleep habits.
- Anatomical factors: People with craniofacial or upper airway characteristics such as a small lower jaw, a large tongue or tonsils, or a neck circumference greater than 17 inches may be at greater risk of developing OSA and may require higher CPAP pressure levels.
- Deviated septum: A deviated septum limits airflow through the nose, so a higher amount of pressure may be needed to keep the upper airway open.
- Body mass index (BMI): People with obesity are more likely to have extra throat tissue that restricts airflow to the lungs. Pressure requirements tend to increase with a person’s weight , so people who lose a significant amount of weight usually need to lower their pressure setting.
- Nasal allergies: Allergies and nasal congestion can make breathing more difficult, thereby reducing oxygen intake. In addition to calibrating pressure settings, a CPAP machine with a humidifier can sometimes help people with allergies. Regularly cleaning filters can also reduce allergen triggers.
- Sleep position: Back sleeping is generally the least favored sleep position for sleep apnea because the pull of gravity puts pressure on the airway. Back sleepers therefore usually require higher pressure settings. Experts recommend side sleeping for people with OSA because it puts less weight on the upper airway.
How to Tell if Your CPAP Pressure Is Properly Set
Proper CPAP pressure levels help alleviate conditions associated with sleep apnea, such as snoring and sleep disturbances. If you are not experiencing better sleep quality after CPAP therapy, you will probably need to consult with your doctor about adjusting your pressure settings.
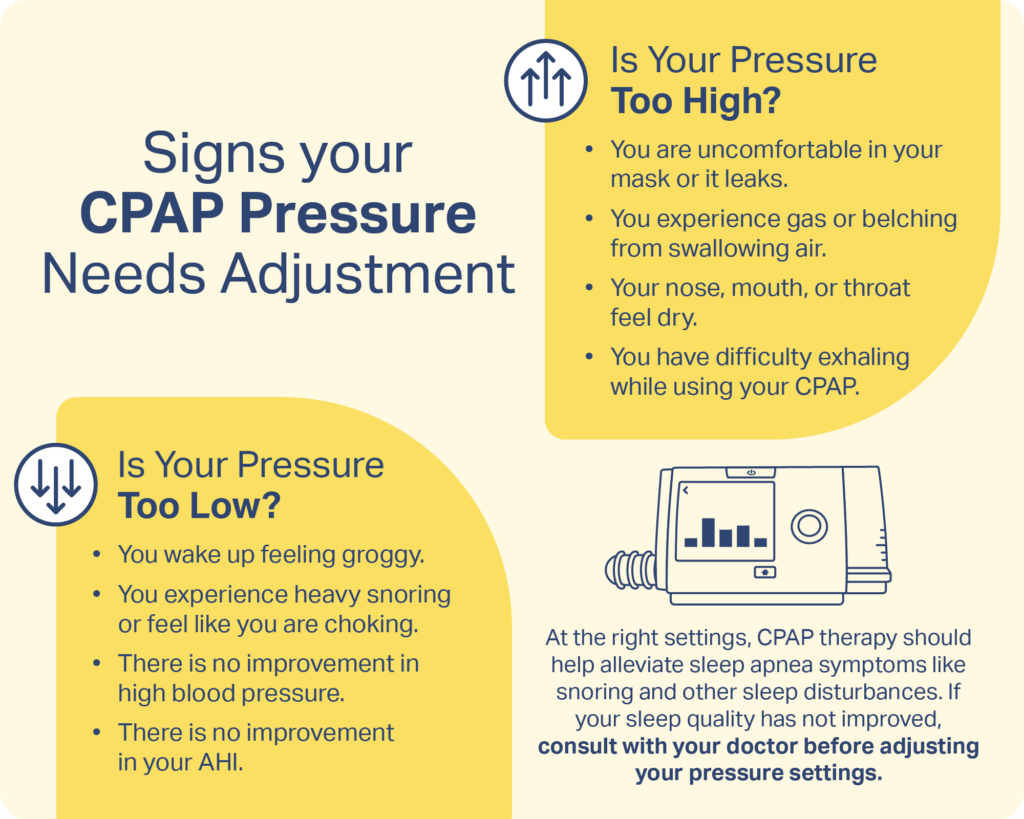
Signs Your CPAP Pressure Is Too Low
If your CPAP pressure is set too low, your machine may not deliver enough airflow to keep your airway fully open throughout the night. As a result, symptoms of obstructive sleep apnea can continue even while you’re using the device. You might also experience the following:
- Waking up feeling groggy or unrefreshed after using a CPAP machine
- Snoring heavily
- Feeling like you’re choking
- Lack of improvement in high blood pressure
If your AHI doesn’t improve once you’ve fully integrated CPAP therapy into your sleep routine, it may also be an indication that the settings should be adjusted.
Signs Your CPAP Pressure Is Too High
When CPAP pressure is set higher than you need, the airflow can feel overwhelming and may cause new discomforts that make therapy harder to tolerate. Excessive pressure can lead to:
- Discomfort
- Struggling to exhale
- Nose and mouth dryness
- Burning sensation in the throat
- Mask leaks
- Fluid in the ears
- Gas or belching from swallowing air (aerophagia)
When to Get Your CPAP Pressure Settings Adjusted
It may be time to have your CPAP pressure settings re-evaluated if you continue to experience sleep apnea symptoms or develop new discomforts while using your machine. Persistent snoring, gasping, daytime sleepiness, or morning headaches can signal that your pressure is too low. On the other hand, difficulty exhaling, excessive mask leaks, aerophagia (air swallowing), or waking with a very dry mouth may suggest your pressure is too high.
You should also talk to your doctor if you’ve recently gained or lost weight, started new medications, or had other health changes that could affect your breathing during sleep. CPAP pressure needs can shift over time, and periodic adjustments ensure your therapy remains safe and effective. A sleep specialist can determine whether a pressure change, mask update, or repeat sleep study is appropriate based on your symptoms and equipment data.
Frequently Asked Questions
What is a normal CPAP pressure setting?
Most CPAP machines operate within a pressure range of 4 to 20 centimeters of water pressure (cm H2O). For many people with obstructive sleep apnea, the average effective pressure falls between 8 and 10 cm H2O, but the “normal” setting varies widely from person to person.
Is it illegal to change CPAP pressure?
No, it’s not illegal to change your CPAP pressure, but it’s strongly discouraged, because CPAP devices are prescription medical equipment. Pressure settings are part of your prescribed treatment, and adjusting them without medical guidance can make your therapy less effective or cause new side effects, such as excessive air pressure, discomfort, or persistent apnea events.
For your safety, pressure changes should always be made by—or in consultation with—a sleep specialist or durable medical equipment provider who can review your symptoms and machine data to determine the right setting.
How do you adjust CPAP pressure?
If you think your pressure level needs adjusting, contact your doctor’s office and bring your CPAP machine to the appointment. Your doctor will evaluate data from the device and make changes as needed. Pressure settings should only be changed under medical supervision.
How do I know if my CPAP pressure is working?
If your CPAP pressure is set correctly, you should wake feeling more rested, experience less daytime sleepiness, and notice improvements in symptoms like loud snoring, gasping, or morning headaches. Your machine’s data can also help indicate whether your therapy is effective. Consistently low AHI numbers and minimal mask leaks are signs that your pressure is working well.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of product specialists, sleep health professionals, and people just like you. Whether you’re searching for the perfect mattress or need expert sleep advice, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
7 Sources
-
Farré, R., Gozal, D., & Montserrat, J. M. (2021). Alternative procedure to individual nasal pressure titration for sleep apnea. Journal of Clinical Medicine, 10(7), 1453.
https://pubmed.ncbi.nlm.nih.gov/33916282/ -
Strohl, K. P. (2022, October). Obstructive sleep apnea. Merck Manual Professional Version.
https://www.merckmanuals.com/professional/pulmonary-disorders/sleep-apnea/obstructive-sleep-apnea -
Yeom, S.W., Kim, M.G., Lee, E.J., Chung, S.K., Kim, D.H., Noh, S.J., Lee, M.H., Yang, Y.N., Lee, C.M., & Kim, J.S. (2021). Association between septal deviation and OSA diagnoses: A nationwide 9-year follow-up cohort study. Journal of Clinical Sleep Medicine. 17(10), 2099–2106.
https://pubmed.ncbi.nlm.nih.gov/34606442/ -
Lankford, D. A., Proctor, C. D., & Richard, R. (2005). Continuous positive airway pressure (CPAP) changes in bariatric surgery patients undergoing rapid weight loss. Obesity Surgery, 15(3), 336–341.
https://pubmed.ncbi.nlm.nih.gov/15826465/ -
Menon, A., & Kumar, M. (2013). Influence of body position on severity of obstructive sleep apnea: A systematic review. ISRN Otolaryngology, Article e670381, 1–7.
https://pubmed.ncbi.nlm.nih.gov/24223313/ -
Kryger, M.H., & Malhotra, A. (2022, August 11). Management of obstructive sleep apnea in adults. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/obstructive-sleep-apnea-overview-of-management-in-adults -
Shafazand, S., & Patel, S. R. (2014). Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension. Journal of Clinical Sleep Medicine, 10(03), 341–343.
https://pubmed.ncbi.nlm.nih.gov/24634635/














































