When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
UPPP Surgery
To resolve nighttime breathing disruptions and alleviate the symptoms of obstructive sleep apnea (OSA), non-surgical interventions like continuous positive airway pressure (CPAP) therapy may be used, as well as lifestyle modifications such as weight management or adjustment of sleep positions. When these treatments are not successful in reducing the symptoms of OSA, doctors may recommend alternative treatments including uvulopalatopharyngoplasty (UPPP), a surgery for sleep apnea.
We discuss this surgery, including its role in treating OSA, its potential benefits and risks, and what to expect before and after the procedure.
What Is UPPP Surgery?
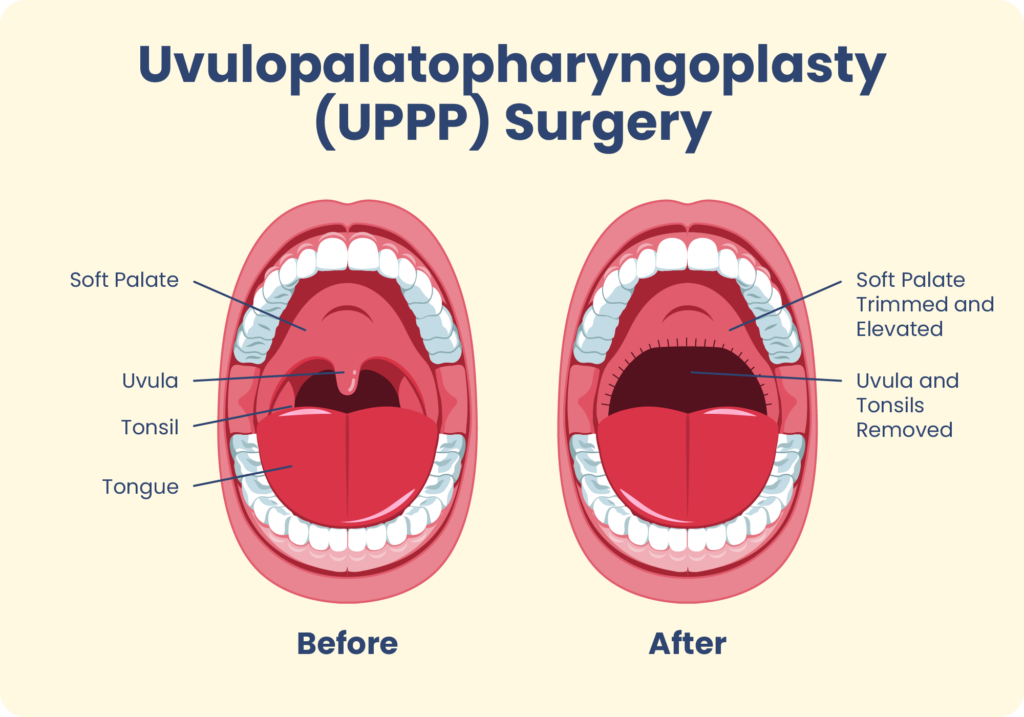
Uvulopalatopharyngoplasty is a surgery that removes and repositions tissue within the airway to make it less likely to collapse and interfere with breathing during sleep. In people with obstructive sleep apnea, abnormal breathing occurs when tissue within the upper airway collapses in on itself, creating an obstruction . UPPP enlarges the airway by altering certain tissue in the throat such as the soft palate, uvula, and tonsils.
- Soft palate: The soft palate is located at the back of the roof of the mouth and is important for breathing, swallowing, and speaking . More than 90% of airway obstructions during sleep may be related to blockages caused by the soft palate.
- Uvula: The soft palate ends at a piece of tissue hanging from the roof of the mouth called the uvula. Because a swollen or enlarged uvula is a frequent cause of airway obstruction, this tissue is often altered or removed during a UPPP.
- Tonsils: The tonsils are tissues found on both sides of the back of the throat that play a role in preventing infection. Larger than normal tonsils are another reason for reduced space in the airway and are a common target of surgery.
Think You May Have Sleep Apnea? Get Help Today

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
Variations of UPPP
A UPPP surgery is composed of several procedures, each targeting specific structures or abnormalities in the airway that contribute to obstructions during sleep.The choice of which procedures to include during UPPP surgery depends on the results of an examination of the mouth and airway as well as an individual’s unique anatomy.
- Tonsillectomy: A tonsillectomy is a procedure in which the tonsils are removed.
- Adenoidectomy: The adenoids are tissues that play a role in preventing infection and are located behind the nose at the top of the throat. When these tissues are removed during surgery, it is called an adenoidectomy.
- Uvulopalatal flap: A uvulopalatal flap procedure involves folding the uvula under the soft palate rather than removing it completely.
- Expansion sphincter pharyngoplasty: This procedure attempts to reinforce the side walls of the airway by removing or repositioning tissues within the throat.
- Palatal advancement pharyngoplasty: During a palatal advancement pharyngoplasty, a doctor removes a portion of the front two-thirds of the roof of the mouth known as the hard palate. This helps adjust the soft palate forward and reduce the risk of airway collapse.
- Relocation pharyngoplasty: Relocation pharyngoplasty repositions tissues in the throat to create tension on the sides of the airway and decrease the likelihood of collapse.
In the past, UPPP focused primarily on removing tissue to expand the airway. Newer variations of UPPP have helped reduce the side effects of the surgery by attempting to reposition or rebuild tissues when possible.
UPPP Surgery for Obstructive Sleep Apnea
Doctors typically recommend uvulopalatopharyngoplasty surgery for the treatment of obstructive sleep apnea when less invasive treatments have been unsuccessful. When surgery is needed, UPPP is the most frequently performed procedure for adults with OSA.
The effectiveness of UPPP varies based on the part of the airway where obstructions occur and the specific surgical procedures performed. While this surgery can often reduce breathing disruptions and other symptoms of OSA, complete resolution of symptoms is uncommon.
UPPP is not commonly performed in children with OSA, as it is more common for children diagnosed with OSA to have the adenoids and tonsils removed to reduce sleep-related breathing problems. However, pediatricians may recommend UPPP in children with certain health conditions, such as Down syndrome.
Because of a lack of research about their effectiveness and the potential for side effects, UPPP and other surgeries for OSA are not recommended for pregnant people .
UPPP Surgery for Snoring
UPPP surgery may be able to reduce snoring because the cause of snoring is often a narrowing of the airway similar to OSA. Although not an initial treatment for snoring, UPPP surgery may be recommended if snoring has not gotten better after less invasive treatments and is caused by anatomic features that can be remedied through surgery.
While most people experience a reduction in snoring after a UPPP, only around half maintain this improvement long-term. UPPP is also an invasive procedure that involves receiving anesthesia and staying in a hospital overnight, so the drawbacks of the procedure often outweigh its benefits for people who snore but do not have sleep apnea.
Benefits and Drawbacks of UPPP Surgery for Obstructive Sleep Apnea
Although past research can help people understand what to expect from surgery, it is important to remember that the specific procedures involved in UPPP depend on an individual’s needs. Because variations of UPPP can affect the surgery’s outcome, it is important to discuss questions about the benefits and drawbacks with a doctor.
Benefits of UPPP
The benefits of UPPP surgery depend on several factors, including the cause of airway obstructions and the procedures involved in the UPPP. In general, around half of people who undergo UPPP experience significantly fewer breathing disruptions during sleep after the operation. Other benefits of UPPP surgery can include:
- Reduced snoring
- Fewer nighttime awakenings
- Less daytime sleepiness
- Lower risk of accidents while driving
- Decreased risk of cardiovascular disease
- Improvements in overall quality of life
Drawbacks of UPPP
Potential side effects of UPPP include post-surgical pain, bleeding, and risk of infection. People who have UPPP surgery may also experience changes in their voice as well as temporary difficulty making certain sounds .
As many as one-third of people develop difficulties related to swallowing and eating after UPPP surgery. Serious side effects of UPPP are uncommon, and the majority of people see improvements in side effects during the first few months after the procedure.
While many people with OSA experience improvements in symptoms after a UPPP surgery, some people find that their OSA comes back over time . Also, UPPP may not eliminate the need for other treatments such as continuous positive airway pressure (CPAP), and people often need to continue these treatments after the procedure.
Is UPPP Covered by Insurance?
Insurance may cover the cost of UPPP, but this depends on a person’s health insurance policy. For people with private medical insurance, contacting the insurance company directly is the best way to learn about what costs may be covered and what may need to be paid out of pocket.
For individuals with Medicare, UPPP is only covered under specific circumstances . Surgery must be needed for the treatment of moderate to severe OSA that is caused by blockages in certain parts of the airway. For coverage to apply, less invasive treatments, such as CPAP therapy, must be attempted first, and a doctor must have a conversation with the patient about the risks and benefits of surgery.
Preparing for UPPP Surgery
Knowing what to expect before and after surgery may reduce anxiety about surgery and can help patients stay informed about their follow-up care plan.
Before UPPP Surgery
Prior to surgery, doctors evaluate a person’s health history and perform testing to determine whether they are a good candidate for uvulopalatopharyngoplasty. The primary care doctor may work directly with a surgeon to determine whether surgery is a safe and beneficial option. Doctors may also use this time to discuss other options for treating OSA and what to expect if a person goes forward with surgery.
An exam of the head and neck as well as imaging tests may be used to find the location of the obstruction and develop a plan for surgery. Because UPPP is performed under general anesthesia, additional tests may be performed to ensure that the surgery can be performed safely.
People scheduled for UPPP surgery should take standard precautions prior to surgery, including telling their doctor about any medications or supplements they take and informing the doctor if they could be pregnant. A doctor, nurse, or another medical professional will review any additional pre-operative instructions and what to expect prior to the day of surgery.
After UPPP Surgery
After waking up from uvulopalatopharyngoplasty, patients are monitored by a medical professional to ensure that the side effects of anesthesia diminish. An overnight hospital stay is often needed to make sure that a person can swallow before they are discharged.
Recovery from UPPP surgery can take two to three weeks, during which time people will be instructed to take any pain medication provided by the doctor, eat soft foods, rinse their mouth after meals, and avoid strenuous activity. During recovery, the symptoms of OSA may temporarily become more severe due to swelling and challenges in using positive airway pressure devices.
A follow-up appointment two to three weeks after surgery may include an examination of the surgical site to check incisions and assess the structure of the airway. The doctor will also ask about any changes in symptoms or new side effects.
After the recovery period, patients typically meet with a sleep specialist for a follow-up sleep study to detect and measure any remaining symptoms of OSA and discuss any need for ongoing treatment, such as continued use of a CPAP device.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
12 Sources
-
Slowick, J. M., Sankari, A., & Collen, J. F. (2022, June 28). Obstructive sleep apnea. In StatPearls. StatPearls Publishing. Retrieved September 8, 2022, from
https://www.ncbi.nlm.nih.gov/books/NBK459252/ -
lwani, M. & Rathee, M. (2022, June 11). Anatomy, head and neck, palate. In StatPearls. StatPearls Publishing. Retrieved September 8, 2022, from
https://www.ncbi.nlm.nih.gov/books/NBK557817/ -
Patel, A., & Kotecha, B. (2019). Minimally invasive radiofrequency surgery in sleep-disordered breathing. Healthcare, 7(3), 97.
https://pubmed.ncbi.nlm.nih.gov/31426606/ -
Schwab, R. J. (2022, January 3). Upper airway imaging in obstructive sleep apnea in adults. In N. Collop & N. L. Muller (Eds.). UpToDate. Retrieved September 8, 2022, from
https://www.uptodate.com/contents/upper-airway-imaging-in-obstructive-sleep-apnea-in-adults -
Pinto, J. A., Godoy, L., Nunes, H., Abdo, K. E., Jahic, G. S., Cavallini, A. F., Freitas, G. S., Ribeiro, D. K., & Duarte, C. (2020). Lateral-expansion pharyngoplasty: Combined technique for the treatment of obstructive sleep apnea syndrome. International Archives of Otorhinolaryngology, 24(1), e107–e11
https://pubmed.ncbi.nlm.nih.gov/31892966/ -
Oh, H., Kim, H. G., Pyo, S., Ji, J. Y., Woo, H., Kim, M., Kim, D. Y., Rhee, C. S., & Kim, H. J. (2020). The clinical efficacy of relocation pharyngoplasty to improve retropalatal circumferential narrowing in obstructive sleep apnea patients. Scientific Reports, 10(1), 2101.
https://pubmed.ncbi.nlm.nih.gov/32034229/ -
Louis, J. & Pien, G. W. (2022, November 28 ). Obstructive sleep apnea in pregnancy. In V. Berghella & N. Collop (Eds.). UpToDate.
https://www.uptodate.com/contents/obstructive-sleep-apnea-in-pregnancy -
Rowley, J. A. (2023, January 6). Snoring in adults. In M. S. Badr (Ed.). UpToDate.
https://www.uptodate.com/contents/snoring-in-adults -
Cheng, A. G. (2022, March). Velopharyngeal insufficiency. Merck Manual Professional Version. Retrieved September 8, 2022, from
https://www.merckmanuals.com/professional/ear,-nose,-and-throat-disorders/oral-and-pharyngeal-disorders/velopharyngeal-insufficiency -
A.D.A.M. Medical Encyclopedia. (2021, June 6). Uvulopalatopharyngoplasty (UPPP). MedlinePlus. Retrieved September 8, 2022, from
https://medlineplus.gov/ency/article/007663.htm -
U.S. Centers for Medicare & Medicaid Services. Surgical treatment of obstructive sleep apnea (OSA). Retrieved September 8, 2022, from
https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?LCDId=34526 -
Olsen, E., Chung, F., & Seet Chuen Ping, E. (2022, August 15). Surgical risk and the preoperative evaluation and management of adults with obstructive sleep apnea. In S. B. Jones & N. Collop (Eds.). UpToDate. Retrieved September 8, 2022, from
https://www.uptodate.com/contents/surgical-risk-and-the-preoperative-evaluation-and-management-of-adults-with-obstructive-sleep-apnea


























































