When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
ASV Machines
- CPAP is the most prescribed treatment for sleep apnea, but some patients with more complex cases or certain types of apnea could benefit from adaptive servo-ventilation (ASV) machines instead.
- ASV is usually prescribed after other PAP therapies are deemed ineffective for a patient.
- Some studies show ASV to be particularly helpful for patients diagnosed with central sleep apnea, but it may pose a risk for patients who have certain heart conditions.
Sleep apnea is a common sleep disorder in the U.S., affecting 10 to 30% of adults. While sleep apnea is commonly treated using positive airway pressure (PAP) therapy – either continuous positive airway pressure (CPAP) or bi-level positive airway pressure (BiPAP) – a newer form of treatment called adaptive servo-ventilation (ASV) may be more effective for some patients.
Adaptive servo-ventilation (ASV) therapy is more commonly used for people who experience central sleep apnea in addition to obstructive sleep apnea (OSA). Below, learn more about how ASV compares to CPAP and BiPAP, how ASV machines work, potential downsides, and which types of patients may benefit from the treatment.
Think You May Have Sleep Apnea? Get Help Today

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
What Is ASV?
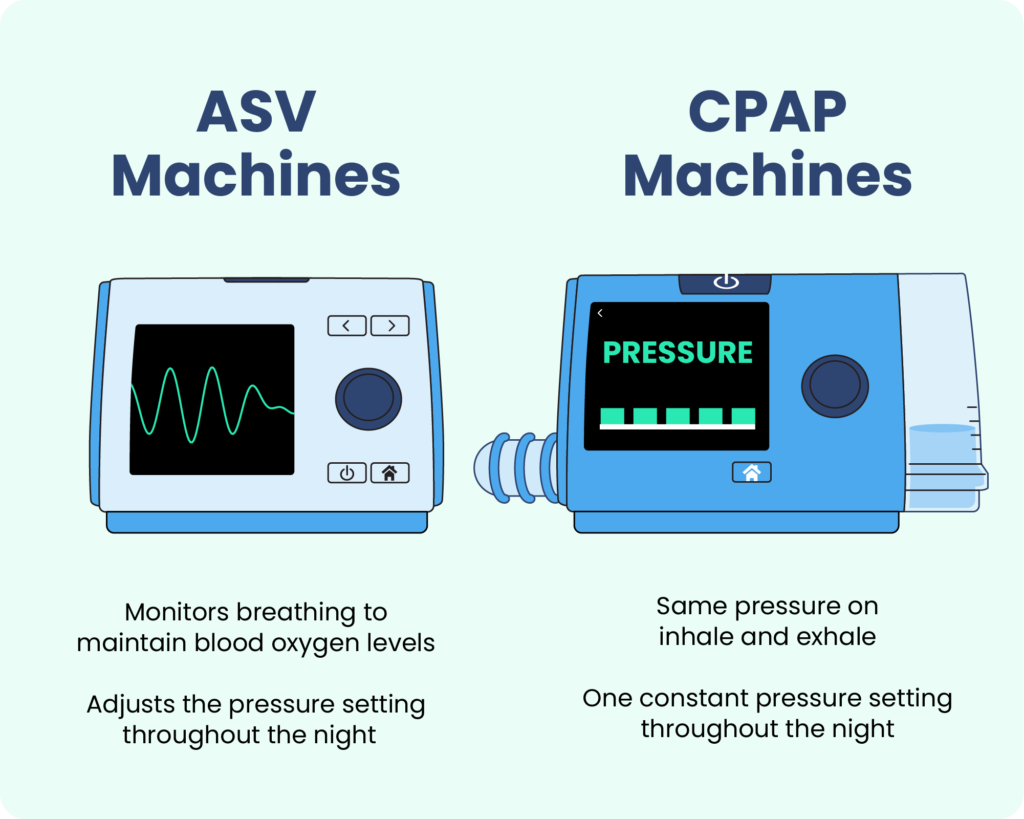
Adaptive servo-ventilation (ASV) machines monitor a person’s breathing while they sleep to deliver customized air pressure that stabilizes breathing . The main difference between ASV and CPAP machines is that ASV machines deliver air pressure dynamically, automatically adjusting according to the person’s breathing patterns, while CPAP machines deliver a set level of air pressure throughout the night. For patients who have central sleep apnea, ASV could be the better treatment option.
While OSA causes apneic events (temporary pauses in breathing) when the airway narrows or becomes blocked, with central sleep apnea, apneic events occur when the brain fails to signal the respiratory muscles to breathe.
Some people with OSA may develop central sleep apnea when using CPAP therapy, which is known as complex sleep apnea, or treatment-emergent central sleep apnea .
Researchers believe that CPAP therapy might contribute to central apneic events in some patients because of reduced carbon dioxide levels. This is when the expanded lungs send a signal to the brain that there is no need to breathe. The problem could also be more complex for people who have congestive heart failure, as well as OSA.
Sometimes, these problems resolve once the patient becomes accustomed to the CPAP device. However, if central apneic events continue, ASV can encourage a more regular breathing pattern. Because it adjusts the air pressure to the appropriate level based on the person’s breathing patterns, it can help avoid brain confusion. In addition, because ASV also delivers air mechanically, it does also help treat OSA events .
How Do ASV Machines Work?
Like CPAP devices, ASV machines consist of three basic parts: a face mask, the machine, and a flexible hose that connects the mask to the machine. Before falling asleep, the person puts the mask on and turns on the machine. ASV masks may either be fitted over the nose and the mouth, or just the nose .
The ASV device monitors a person’s breathing throughout the night. If a person’s breathing slows down, the machine responds with enough pressure to return them to normal breathing levels. Once their breathing goes back to normal, the ASV machine lowers the pressure, but may still provide a baseline level of support to make it easier for the person to breathe normally.
This method helps regularize breathing for people who respond poorly to CPAP therapy . The variability in air pressure may also relieve some of the discomfort people feel with CPAP therapy .
How Does ASV Compare to Other PAP Therapy?
Although ASV is a similar form of therapy to other PAP treatments, the main difference is that ASV uses an algorithm to adjust to the patient’s breathing, while the others deliver a pre-set amount of air pressure.
ASV vs. CPAP
As opposed to ASV machines, continuous positive airway pressure (CPAP) devices deliver a set amount of air pressure continuously throughout the night.
CPAP is typically the first-line of treatment prescribed for patients with OSA, while ASV is usually only suggested if the patient has challenges with CPAP and/or BiPAP, or if central sleep apnea is diagnosed.
ASV vs. BiPAP
Just as with CPAP, the main difference between ASV and bi-level positive airway pressure (BiPAP) is that ASV machines adapt to a patient’s breathing while BiPAP machines use preset levels.
They do have a similarity, however, as both ASV and BiPAP machines provide a backup respiratory rate, which helps maintain breathing during central apneic events. ASV machines differ in that this backup respiratory rate can be personalized based on ongoing feedback from the person’s breathing patterns.
ASV vs. APAP
Automatic positive airway pressure (APAP) may seem the most similar to ASV since they both adjust based on the patient’s breathing level. However, the key difference is that ASV is a much more advanced machine that adapts through continuous monitoring to offer more precise air pressure at each given moment. An APAP machine also makes pressure adjustments, but it’s within a set range, meaning air is always flowing, just at different levels.
As far as what they are used for, APAP is an acceptable alternative treatment to CPAP for patients with uncomplicated OSA. ASV, on the other hand, is a last line of treatment once other PAP therapies have been exhausted, or for more complicated cases of OSA or central sleep apnea.
What Are the Potential Side Effects of ASV?
While ASV therapy can be effective, it is not recommended for everyone. Specifically, there are higher risks for people with a certain type of congestive heart failure that affects pumping, called reduced ejection fraction. For this reason, experts do not recommend using ASV to treat central sleep apnea in people with this type of heart failure.
Similar to CPAP machines, ASV machines can cause some side effects and discomfort, such as:
- Aerophagia (air swallowing)
- Congestion
- Difficulty sleeping due to mask discomfort
- Dry mouth
- Eye irritation
- Mask leak
- Mouth leak
- Nostril irritation
- Skin irritation or creasing from the mask
Using a humidifier may decrease some symptoms, like dry mouth.
Compared to CPAP therapy, ASV machines are generally less likely to cause feelings of claustrophobia when exhaling against pressurized air. This feeling is a common reason why people stop using CPAP therapy.
There is relatively little research on the potential risks and side effects of ASV machines . Companies may also use proprietary algorithms to determine airflow rates, making it difficult to compare across models.
Who Is ASV Best For?
ASV was originally developed for people with Cheyne-Stokes respirations, a condition linked to heart failure that involves hyperventilation followed by lapses in breathing . ASV therapy is also used to treat sleep-disordered breathing in people with:
- Central sleep apnea, including CSA due to stroke, kidney failure, neurological conditions, or opioid use
- Complex sleep apnea, or treatment-emergent central sleep apnea, which arises during OSA treatment
- Mixed sleep apnea, involving obstructive and central apneic events
ASV therapy has proven to be more effective than CPAP therapy in cases of drug-induced sleep-disordered breathing, which can affect people taking opioids for pain management or with former drug abuse. There is also interest in using ASV therapy to improve breathing for people with CSA due to neurological disorders. ASV therapy can also be effective for people who do not respond to CPAP treatment, such as those who have both chronic complex insomnia and OSA.
Typically, CPAP is attempted before ASV. ASV therapy is more expensive, and CPAP therapy is often successful at treating OSA as long as people continue to use the device . That said, many people find ASV machines to be more comfortable, which may make it easier to adhere to their treatment.
Whatever type of device you are using to manage your sleep apnea, it is best to consult with your doctor about any discomfort you are feeling. They can adjust your machine settings, or recommend a different type of device to help you breathe and sleep easier through the night.
Frequently Asked Questions
How do you clean an ASV machine?
To clean an ASV machine, follow the manufacturer’s guidance. In general, you can use mild soap and warm water daily on the mask and humidifier chamber, and a damp cloth to wipe down the machine. You should also do a deep cleaning weekly on detachable parts including hosing using mild soap or a white vinegar solution, followed by air drying. Make sure your machine is completely dry before using it.
Do you need a prescription for an ASV machine?
Yes, you will need a prescription in order to purchase or rent an ASV machine, since it’s considered a Class II medical device as per the FDA.
How much does an ASV machine cost?
The cost of ASV machines vary by model, and your out-of-pocket cost is determined by your insurance coverage. Because of their complexity, you can expect ASV machines to have a higher price tag than other PAP devices. Depending on your financial situation, they can cost anywhere from $1,000 to $4,000.
Who sets the pressure levels for an ASV machine?
The initial pressure setting on your ASV machine is done by your doctor or sleep technologist. However, once you begin using it at home, the machine uses an algorithm to monitor your breathing during sleep so it can make air pressure adjustments automatically in real time.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
18 Sources
-
Kline, L. R. (2022, April 1). Clinical presentation and diagnosis of obstructive sleep apnea in adults. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-obstructive-sleep-apnea-in-adults -
National Heart, Lung, and Blood Institute. Sleep apnea – what is sleep apnea? www.nhlbi.nih.gov. Published March 24, 2022.
https://www.nhlbi.nih.gov/health-topics/sleep-apnea -
Jaffuel, D., Philippe, C., Rabec, C., Mallet, J. P., Georges, M., Redolfi, S., Palot, A., Suehs, C. M., Nogue, E., Molinari, N., & Bourdin, A. (2019). What is the remaining status of adaptive servo-ventilation? The results of a real-life multicenter study (OTRLASV-study): Adaptive servo-ventilation in real-life conditions. Respiratory Research, 20(1), 235.
https://pubmed.ncbi.nlm.nih.gov/31665026/ -
Sharma, B. K., Bakker, J. P., McSharry, D. G., Desai, A. S., Javaheri, S., & Malhotra, A. (2012). Adaptive servoventilation for treatment of sleep-disordered breathing in heart failure: A systematic review and meta-analysis. Chest, 142(5), 1211–1221.
https://pubmed.ncbi.nlm.nih.gov/22722232/ -
Zhang, J., Wang, L., Guo, H. J., Wang, Y., Cao, J., & Chen, B. Y. (2020). Treatment-emergent central sleep apnea: A unique sleep-disordered breathing. Chinese Medical Journal, 133(22), 2721–2730.
https://pubmed.ncbi.nlm.nih.gov/33009018/ -
Cowie, M. R., Woehrle, H., Oldenburg, O., Damy, T., van der Meer, P., Erdman, E., Metra, M., Zannad, F., Trochu, J. N., Gullestad, L., Fu, M., Böhm, M., Auricchio, A., & Levy, P. (2015). Sleep-disordered breathing in heart failure – current state of the art. Cardiac Failure Review, 1(1), 16–24.
https://pubmed.ncbi.nlm.nih.gov/28785426/ -
Cantero, C., Adler, D., Pasquina, P., Uldry, C., Egger, B., Prella, M., Younossian, A. B., Poncet, A., Soccal-Gasche, P., Pepin, J. L., & Janssens, J. P. (2020). Adaptive servo-ventilation: A comprehensive descriptive study in the Geneva Lake area. Frontiers in Medicine, 7, 105.
https://pubmed.ncbi.nlm.nih.gov/32309284/ -
Pépin, J. L., Woehrle, H., Liu, D., Shao, S., Armitstead, J. P., Cistulli, P. A., Benjafield, A. V., & Malhotra, A. (2018). Adherence to positive airway therapy after switching from CPAP to ASV: A big data analysis. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine, 14(1), 57–63.
https://pubmed.ncbi.nlm.nih.gov/29198291/ -
Krakow, B., McIver, N. D., Ulibarri, V. A., Krakow, J., & Schrader, R. M. (2019). Prospective randomized controlled trial on the efficacy of continuous positive airway pressure and adaptive servo-ventilation in the treatment of chronic complex insomnia. EClinicalMedicine, 13, 57–73.
https://pubmed.ncbi.nlm.nih.gov/31517263/ -
Pinto, V. L., & Sharma, S. (2021). Continuous positive airway pressure. StatPearls.
https://pubmed.ncbi.nlm.nih.gov/29489216/ -
Asp K. Pros and Cons of Adaptive Servo-Ventilation (ASV) for Sleep Apnea – American Association of Sleep Technologists. American Association of Sleep Technologists. Published November 17, 2022.
https://aastweb.org/pros-and-cons-of-adaptive-servo-ventilation-asv-for-sleep-apnea/ -
Fashanu OS, Budhiraja R, Batool-Anwar S, Quan SF. Titration studies overestimate continuous positive airway pressure requirements in uncomplicated obstructive sleep apnea. Journal of Clinical Sleep Medicine. 2021;17(9):1859-1863. doi:https://doi.org/10.5664/jcsm.9316
https://jcsm.aasm.org/doi/10.5664/jcsm.9316 -
Patel A, Perez I, Rabiei-Samani S. What Is Adaptive Servo-Ventilation (ASV)?. Am J Respir Crit Care Med. 2021;204(2):P3-P4. doi:10.1164/rccm.2042P3
https://www.thoracic.org/patients/patient-resources/resources/adaptive-servo-ventilation-asv.pdf -
Selim, B., & Ramar, K. (2016). Advanced positive airway pressure modes: Adaptive servo ventilation and volume assured pressure support. Expert Review of Medical Devices, 13(9), 839–851.
https://pubmed.ncbi.nlm.nih.gov/27478974/ -
Rudrappa, M., Modi, P., & Bollu, P. C. (2021). Cheyne Stokes respirations. In StatPearls. StatPearls Publishing.
https://pubmed.ncbi.nlm.nih.gov/28846350/ -
Javaheri S, Harris N, Howard J, Chung E. Adaptive servoventilation for treatment of opioid-associated central sleep apnea. J Clin Sleep Med. 2014;10(6):637-643. Published 2014 Jun 15. doi:10.5664/jcsm.3788
https://pmc.ncbi.nlm.nih.gov/articles/PMC4031404/ -
Mehrtash, M., Bakker, J. P., & Ayas, N. (2019). Predictors of continuous positive airway pressure adherence in patients with obstructive sleep apnea. Lung, 197(2), 115–121.
https://pubmed.ncbi.nlm.nih.gov/30617618/ -
American Academy of Sleep Medicine. (2018, October 19). FDA reclassifies positive airway pressure as a Class II medical device.
https://aasm.org/fda-reclassifies-positive-aiway-pressure-class-ii-medical-device/




























































