When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Sleep Apnea and Heart Disease
- Sleep apnea is linked to an increased risk of heart disease.
- Obstructive sleep apnea can lead to high blood pressure and strain the heart.
- Treating sleep apnea can improve heart health and reduce the risk of cardiovascular issues.
Sleep apnea is a sleep disorder in which a person repeatedly stops breathing during sleep. A narrowed or blocked airway restricts air from getting to the lungs, often causing a person to snore loudly or gasp for air. These pauses in breathing can occur a few times a night or, in severe cases, more than once every two minutes during sleep.
Beyond feeling tired during the day, repeated pauses in breath deprive the lungs of oxygen and cause significant stress on the body. Sleep apnea is associated with a range of serious health complications, including coronary heart disease, heart failure, stroke, and an irregular heartbeat.
The Link Between Sleep Apnea and Heart Disease
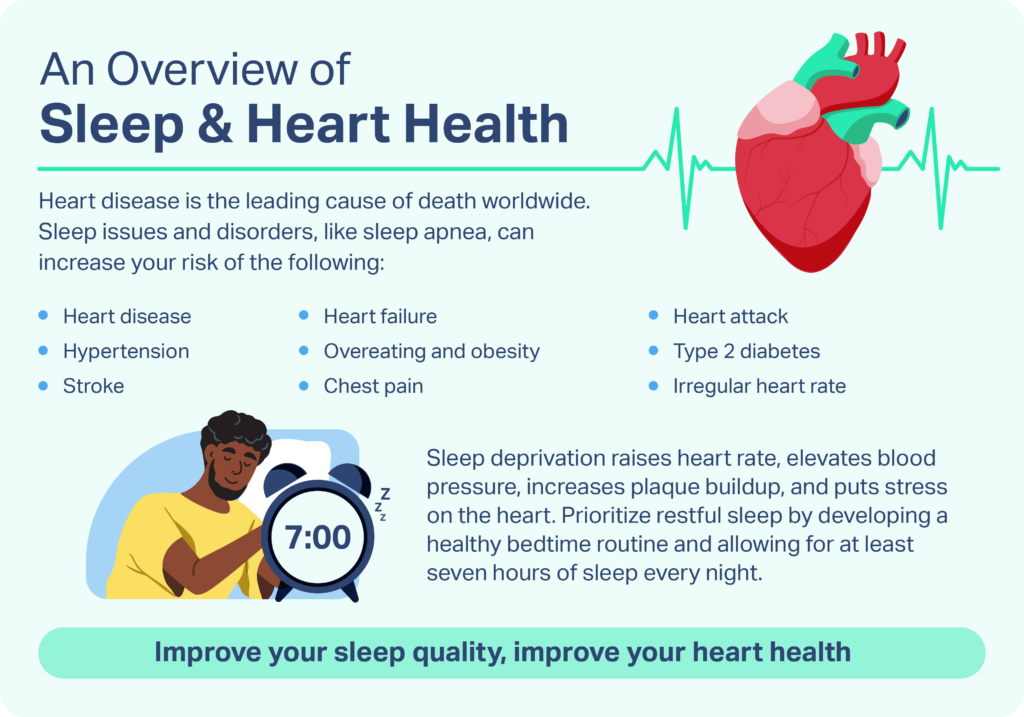
Heart disease is the leading cause of death in the United States and globally . Several behaviors increase the risk of heart disease, including eating an unhealthy diet, not getting enough physical activity, drinking too much alcohol, and smoking. Health conditions that increase the risk of heart disease include high blood pressure, unhealthy cholesterol levels, diabetes, and obesity.
Untreated sleep apnea also significantly increases the risk of heart arrhythmias and cardiovascular disease. It’s estimated that patients with sleep apnea are 2-4 times more likely to develop heart arrhythmias (abnormal heart rhythms) than people without this condition. Sleep apnea increases the risk of heart failure by 140% and the risk of coronary heart disease by 30%.
Around 34% of men and 17% of women live with obstructive sleep apnea (OSA), the most common form of sleep apnea. Researchers estimate that over 80% of cases of moderate to severe OSA are undiagnosed. This means that millions of people are living with some of the consequences of sleep apnea, but don’t know they have this disorder.
Think You May Have Sleep Apnea? Get Help Today

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
How Insufficient Sleep Impacts Heart Health
Insufficient or fragmented sleep is common in patients with sleep apnea, and regularly missing sleep can negatively affect heart health. One of the many important roles of sleep is to allow the body to rest and recuperate. Heart rate and blood pressure drop during sleep as breathing becomes stable and regular.
Not getting enough sleep as a result of conditions like OSA means not giving the heart and cardiovascular system this important recovery time. Chronic sleep deprivation has been linked to increased risk for hypertension, heart disease, heart attacks, and stroke.
Sleep Apnea’s Effects on the Cardiovascular System
The repetitive pauses in breathing that characterize sleep apnea can stress and potentially damage not only the heart, but the whole cardiovascular system. While researchers are continuing to learn about the ways in which sleep apnea affects the cardiovascular system and contributes to heart disease, several biological pathways have been suggested.
Compounded Risks of Sleep Apnea and Obesity
Research suggests that obesity may play an important role in the development of both sleep apnea and heart disease. It is important to keep in mind that sleep apnea alone, with or without obesity, can increase the risk for heart disease. Sleep apnea and obesity independently increase the risk of health conditions that negatively affect heart health, like hypertension (high blood pressure), unhealthy cholesterol levels, and diabetes.
Obesity is a common cause of sleep apnea, often related to increased deposits of fat in the neck that narrow or block the upper airway during sleep. Researchers have found that even a 10% increase in body weight increases the risk of OSA by six-fold. While 60 to 90% of people with sleep apnea also have obesity, only around 30% of people diagnosed with obesity have sleep apnea.
Activating the Sympathetic Nervous System
Each time a person with sleep apnea stops breathing, the level of oxygen in the blood decreases. As the body becomes deprived of oxygen, specialized cells — called chemoreceptors — detect these changes and activate the sympathetic nervous system to respond, which is the part of the nervous system responsible for reacting to stressful or dangerous situations. The sympathetic nervous system triggers the body to gasp for air, which sometimes wakes a person out of sleep.
The sympathetic nervous system also responds to a low level of oxygen by constricting blood vessels and increasing heart rate and blood pressure. As the pauses in breath continue throughout the night, repetitive changes in blood pressure may lead to hypertension or make existing hypertension worse.
Changes in Pressure Within the Chest
When a person with obstructive sleep apnea (OSA) attempts to breathe, they inhale against a narrowed or closed upper airway. These unsuccessful, forced inhalations can cause substantial changes in pressure within the chest cavity. Over time, these repetitive changes in intrathoracic pressure can damage the heart. Intrathoracic pressure changes can lead to atrial fibrillation (an irregular, often rapid heartbeat), problems with blood flow to the heart, and even heart failure.
Oxidative Stress
After each pause in breath, a person with sleep apnea once again inhales successfully. This inhale brings much-needed oxygen back into the lungs, blood, and body tissues. Unfortunately, frequent changes in oxygen levels can cause significant stress on the body, called oxidative stress. Oxidative stress can promote systemic inflammation, as well as neurochemical and physiological reactions that increase the risk of heart disease.
How To Reduce the Risk of Heart Disease
Given the significant health consequences of untreated sleep apnea, it’s important to know when it’s time to reach out to a doctor. Common signs and symptoms of sleep apnea include:
- Frequent, loud snoring or gasping during sleep
- Reduced breathing or pauses in breathing during sleep
- Daytime sleepiness and fatigue
- Difficulty maintaining attention and concentration
- Dry mouth or headaches when waking
- Sexual dysfunction or decreased libido
- Waking up often at night to urinate
Primary care doctors or sleep specialists are all good resources if you’re concerned about having sleep apnea. Diagnostic tests for sleep apnea often include a comprehensive sleep evaluation and polysomnography to diagnose or rule out this serious condition. If a person is diagnosed, treatment depends on the type of sleep apnea detected and may include:
- Lifestyle changes: Doctors may begin by informing patients about lifestyle changes that may reduce the severity of this condition. Weight loss, exercise, limiting alcohol, quitting smoking, and even changing your sleeping position may be helpful.
- Positive airway pressure (PAP) devices: PAP devices pump air through the airway, preventing the upper airway from collapsing during sleep.
- Mouthpieces and oral appliances: Oral appliances reduce disordered breathing by changing the position of the jaw, tongue, or other part of the body that’s constricting the airway.
- Mouth and throat exercises: Depending on the cause of a person’s sleep apnea, special exercises of the mouth and throat may help tone these muscles, making them less likely to interfere with breathing during sleep.
- Surgery: Surgery for sleep apnea may involve changing parts of the body that cause airway constriction or implanting devices that causes tightening of the muscles around the airway.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
10 Sources
-
Centers for Disease Control and Prevention. (2020, October 30). Leading causes of death.
https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm -
World Health Organization. (2017, May 17). Cardiovascular diseases (CVDs).
https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) -
National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. (2019, December 9). Know your risk for heart disease. Centers for Disease Control and Prevention.
https://www.cdc.gov/heart-disease/risk-factors/index.html -
Drager, L. F., McEvoy, R. D., Barbe, F., Lorenzi-Filho, G., Redline, S., & INCOSACT Initiative (International Collaboration of Sleep Apnea Cardiovascular Trialists) (2017). Sleep Apnea and Cardiovascular Disease: Lessons From Recent Trials and Need for Team Science. Circulation, 136(19), 1840–1850.
https://pubmed.ncbi.nlm.nih.gov/29109195/ -
Javaheri, S., Barbe, F., Campos-Rodriguez, F., Dempsey, J. A., Khayat, R., Javaheri, S., Malhotra, A., Martinez-Garcia, M. A., Mehra, R., Pack, A. I., Polotsky, V. Y., Redline, S., & Somers, V. K. (2017). Sleep Apnea: Types, Mechanisms, and Clinical Cardiovascular Consequences. Journal of the American College of Cardiology, 69(7), 841–858.
https://pubmed.ncbi.nlm.nih.gov/28209226/ -
Kapur, V., Blough, D. K., Sandblom, R. E., Hert, R., de Maine, J. B., Sullivan, S. D., & Psaty, B. M. (1999). The medical cost of undiagnosed sleep apnea. Sleep, 22(6), 749–755.
https://academic.oup.com/sleep/article-lookup/doi/10.1093/sleep/22.6.749 -
Grandner, M. A., Alfonso-Miller, P., Fernandez-Mendoza, J., Shetty, S., Shenoy, S., & Combs, D. (2016). Sleep: important considerations for the prevention of cardiovascular disease. Current opinion in cardiology, 31(5), 551–565.
https://journals.lww.com/co-cardiology/Abstract/2016/09000/Sleep__important_considerations_for_the_prevention.12.aspx -
Ramar, K., & Caples, S. M. (2010). Cardiovascular consequences of obese and nonobese obstructive sleep apnea. The Medical clinics of North America, 94(3), 465–478.
https://pubmed.ncbi.nlm.nih.gov/20451027/ -
Pillar, G., & Shehadeh, N. (2008). Abdominal fat and sleep apnea: the chicken or the egg?. Diabetes care, 31 Suppl 2(7), S303–S309.
https://diabetesjournals.org/care/article/31/Supplement_2/S303/24789/Abdominal-Fat-and-Sleep-ApneaThe-chicken-or-the -
Somers et al., American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, American Heart Association Stroke Council, American Heart Association Council on Cardiovascular Nursing, & American College of Cardiology Foundation (2008). Sleep apnea and cardiovascular disease: an American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation, 118(10), 1080–1111.
https://linkinghub.elsevier.com/retrieve/pii/S0735109708016999


























































