Napping: Benefits and Tips
- A midday nap can enhance alertness, mood, memory, and reduce stress.
- Choose a comfortable, quiet spot and time your naps well to avoid grogginess.
- The ideal nap length, between 20 and 30 minutes, should help you wake up feeling refreshed without falling into deep sleep.
- Excessive daytime sleepiness may indicate a sleep disorder and should be evaluated by a professional.
A nap is a short period of sleep that usually occurs during the day. For many adults, naps can help to maintain alertness or overcome daytime fatigue.
Nap needs and the benefits of napping can vary among individuals. Knowing the facts about napping can help determine whether to take naps, and tips for better naps can enable healthier napping habits.
Looking to improve your sleep? Try upgrading your mattress.
Benefits of Naps
Naps can deliver a number of benefits. Brief naps can be restorative and reduce fatigue during the day. After a night of insufficient sleep, a nap may counteract daytime drowsiness . Naps can be particularly beneficial for shift workers who struggle to get enough sleep and have to be alert at irregular times.
A short daytime snooze may also boost workplace performance . A nap can improve cognitive functions such as memory, logical reasoning, and the ability to complete complex tasks.
Some studies have found that physical performance can also improve after napping . Athletes may experience improved endurance, reaction times, and cognitive performance if they take a daytime nap.
Napping may provide other health benefits. One observational study found that napping one or two times a week was associated with a lower risk of cardiovascular problems , such as heart attack, stroke, or heart disease. However, more research is needed to understand the complex ways that the frequency and duration of naps affect heart health.
Napping may also reduce the impacts of insufficient sleep. For example, a small trial found evidence that naps relieved stress and supported the immune system in people whose sleep was limited the night before.
Additionally, naps may contribute to the well-being of specific groups of people. For instance, a study of people diagnosed with intracranial aneurysms found that regularly napping was associated with a lowered risk of a rupture of the aneurysm.
What Are the Drawbacks of Napping?
Although there are a variety of benefits to napping, naps may have drawbacks for certain people. For example, for older adults, napping during the day is associated with self-reported sleep problems such as waking up frequently during the night.
Napping may have other negative health impacts. One study in China found that napping for more than 90 minutes was associated with high blood pressure
in middle-aged and older women. Another study of older Chinese people found that taking naps longer than 30 minutes was correlated with a higher frequency of non-alcoholic fatty liver disease
.
An analysis of multiple studies found that napping for more than 60 minutes a day was associated with an increased risk of developing type 2 diabetes
. Another large study of people living in France found napping to be more common
in people living with anxiety or depression, obesity, high blood pressure, and type 1 and type 2 diabetes.
To date, it is not clear how exactly naps affect health. Much remains unknown about the relationship between naps and nighttime sleep, and how the frequency or length of naps influences well-being for different people.
How Sleep Works During Nap Time
Whether at night or during the day, sleep unfolds in a series of stages that make up a sleep cycle.
- Stage 1: Stage 1 is the lightest and briefest stage of sleep, lasting only one to seven minutes.
- Stage 2: Stage 2 follows stage 1 and lasts about 10 to 25 minutes. During stage 2 sleep, the muscles relax, and body functions slow. However, sleep in this stage is still relatively light.
- Stage 3: Stage 3 is a deeper, more restorative stage of sleep, and it can be difficult to wake up while in this stage. Stage 3 usually lasts between 20 and 40 minutes.
- Rapid eye movement (REM): During REM sleep, the body’s muscles are temporarily paralyzed, and the eyes move quickly under closed eyelids. Dreaming tends to take place during REM sleep.
When sleep periods last several hours, the body cycles through these stages several times. During a nap, though, there is not enough time to go through multiple sleep cycles.
In fact, during a short nap, a person may not be asleep long enough to spend much, if any, time in stage 3 or REM sleep. This can actually make it easier to wake up refreshed from a quick nap.
Longer naps, such as those lasting more than 30 minutes, can cause the sleeper to enter deep sleep, and deep sleep may start even sooner in people who are sleep deprived. Grogginess often results from being woken up during deep sleep.

Tips to Take the Best Nap
To get the full benefits from nap time, it is important to consider where, when, and how long to nap. These and other factors can influence how a person will feel after waking up from a nap.
How Long Should a Nap Be?
In general, the best nap length for adults is about 20 minutes and no longer than 30 minutes. Sleeping for 20 minutes allows the napper to get a bit of light sleep to boost alertness without entering into deep sleep. Waking up from deep sleep can cause grogginess and actually worsen sleepiness.
In some cases, a longer nap of around an hour and a half may also be beneficial. This length of time allows the body to cycle through the stages of sleep and avoids interrupting deep sleep. This type of longer nap may be especially helpful for emergency workers and shift workers who are trying to avoid fatigue.
Napping may be too much if it interferes with sleep at night. Sometimes a nap of 90 minutes or so can be refreshing, but it may be problematic if it happens too late in the day. Dependency on naps, rather than consistent nighttime sleep, can contribute to fragmented sleep or sleep disorders such as insomnia.
However, naps may not affect everyone in the same way. Some research suggests that napping affects nighttime sleep primarily in older adults rather than young and middle-aged adults.
When to Take a Nap
Experts typically recommend that adults take naps eight or more hours before bedtime. For most people, that means napping before 3 p.m. Napping too late in the day may contribute to nighttime sleep problems.
For some people, naps may feel natural or even necessary after lunchtime. This is sometimes known as the post-lunch dip. While eating lunch may play a role in afternoon sleepiness, the post-lunch dip is linked to circadian rhythm. Circadian rhythm is the body’s internal clock that follows a 24-hour cycle. Within this cycle are two peak periods for sleepiness. The greatest peak is during the night, and the second one falls in the early afternoon.
Where to Take a Nap
A good sleep environment is cool, quiet, and dark. Having a comfortable nap setting can help prevent unwanted interruptions or awakenings.
For people who work from home, a bedroom is likely a good place for a short snooze since it is already set up to promote sleep. Adding blackout curtains or a white noise machine to block out distractions may help both at night and during daytime naps.
In an office setting, accessories such as earplugs or an eye mask can reduce disruptions during nap time. When possible, naps should be taken in a space where interruptions are unlikely to occur. Some offices may even have nap pods or other quiet areas for relaxation or a short period of restorative sleep.
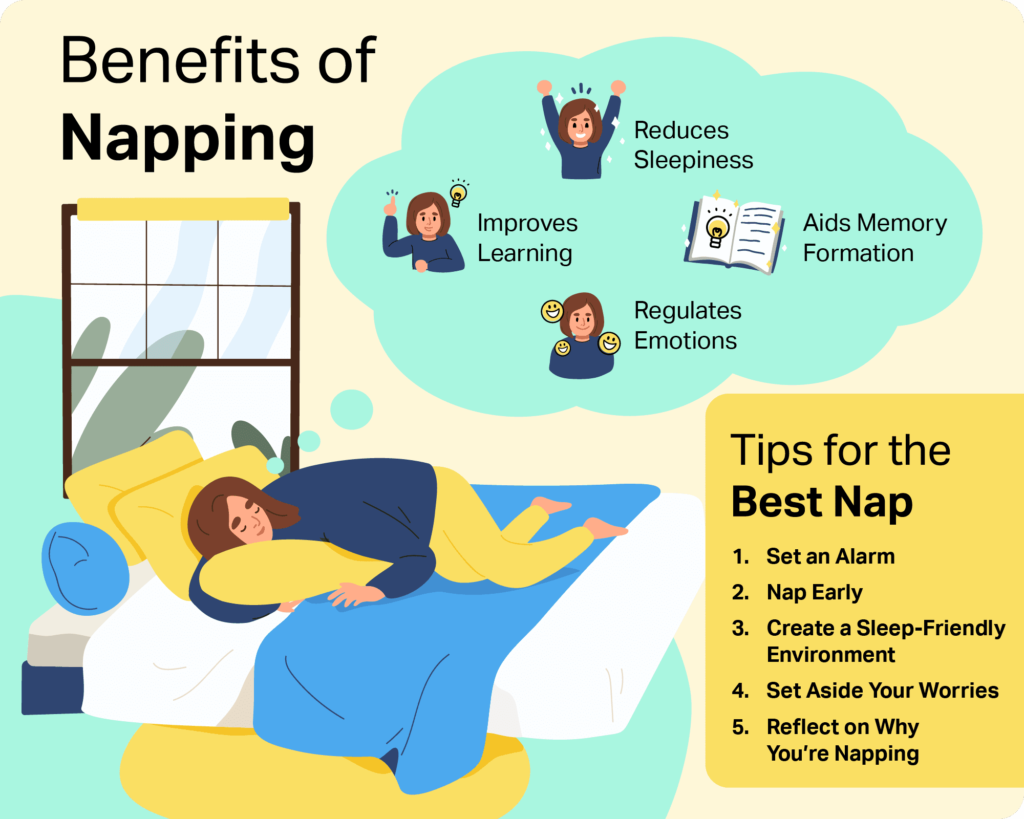
Remember to Set an Alarm
Before dozing off during nap time, set an alarm for the desired nap length, which should generally be around 20 minutes.
When the alarm goes off, do not hit snooze to keep sleeping since this can risk entering deeper sleep. Setting a second alarm to go off shortly after the first one may help to avoid napping for too long.
Try to get up as soon as the alarm sounds and then stretch or walk around to shake off any post-nap sleepiness.
Consider Caffeine Naps
People taking a nap to get a boost of energy may benefit from drinking caffeine before napping. The brain and body feel the impact of caffeine about 30 minutes after it is consumed, so having caffeine right before a short nap may increase alertness after waking up.
Frequently Asked Questions About Naps
How Much Napping Is Too Much?
In many cases, napping longer than 30 minutes can result in grogginess and diminished performance after waking up. In other words, napping too long can undermine the purpose of the nap. For any individual, it is important to reflect on daily energy levels and the duration and frequency of naps. If daytime sleepiness is negatively affecting you on a regular basis, it may indicate a need to change sleep habits.
What Is the Best Time of Day to Nap?
For most people, the best time to take a nap is either just before or during the post-lunch dip. The post-lunch dip is the period of decreased alertness and productivity often experienced after a midday meal. A brief snooze around this time may help reduce afternoon sleepiness without interfering with nighttime sleep.
What Is the Difference Between Naps for Children and Adults?
Newborns, infants, and toddlers require more sleep than adults, and it is common for them to have sleep periods during the day that supplement the sleep they get at night. Babies may take one or more naps per day, depending on their age, while toddlers tend to take only one nap each day. Similar to adults, toddlers’ nap times should occur well before bedtime.
Also like adults, children’s nap environments should be free of noise, excess light, or other distractions. Over time, children may reduce the time they spend napping or stop napping altogether.
Should I Change My Napping Habits?
Your current napping habits may not fit perfectly with expert recommendations, but that does not necessarily mean the way that you nap is wrong. You should only change your napping habits if you are having problems with your nightly sleep or your daily energy level.
If you are not a regular napper, change may not be necessary. If you are able to function well each day without a nap, then napping may not be something you need to incorporate into your daily schedule.
How Do I Start Napping?
You may have to experiment with the timing, duration, and location of your nap. Consider keeping a nap diary where you can record your sleepiness or fatigue levels before and after your nap, as well as where, when, and how long you napped. These recordings can help you track what type of nap is most effective for you.
When Should I Talk to a Doctor?
Excessively napping can also be a symptom of a mental health disorder such as anxiety or depression. Contact your doctor if you are experiencing other related symptoms, such as low mood, change in weight or eating habits, or a lack of interest in activities that you would normally enjoy.
Falling asleep unexpectedly or at unwanted times is different from napping and may be a sign of an underlying condition, such as excessive daytime sleepiness or narcolepsy. If you are struggling to get enough sleep at night or are unable to stay awake during normal daytime hours, talk with your health care provider.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
13 Sources
-
Goldstein, C. A. (2022, April 5). Jet lag. In R. Benca (Ed.). UpToDate., Retrieved July 20, 2022, from
https://www.uptodate.com/contents/jet-lag -
National Heart, Lung, and Blood Institute. (n.d.). Sleep deprivation and deficiency., Retrieved July 20, 2022, from
https://www.nhlbi.nih.gov/health/sleep-deprivation -
Souabni, M., Hammouda, O., Romdhani, M., Trabelsi, K., Ammar, A., & Driss, T. (2021). Benefits of daytime napping opportunity on physical and cognitive performances in physically active participants: A systematic review. Sports Medicine, 51(10), 2115–2146.
https://pubmed.ncbi.nlm.nih.gov/34043185/ -
Häusler, N., Haba-Rubio, J., Heinzer, R., & Marques-Vidal, P. (2019). Association of napping with incident cardiovascular events in a prospective cohort study. Heart (British Cardiac Society), 105(23), 1793–1798.
https://pubmed.ncbi.nlm.nih.gov/31501230/ -
Faraut, B., Nakib, S., Drogou, C., Elbaz, M., Sauvet, F., De Bandt, J. P., & Léger, D. (2015). Napping reverses the salivary interleukin-6 and urinary norepinephrine changes induced by sleep restriction. The Journal of Clinical Endocrinology and Metabolism, 100(3), E416–E426.
https://pubmed.ncbi.nlm.nih.gov/25668196/ -
Kang, H., Feng, X., Zhang, B., Guo, E., Wang, L., Qian, Z., Liu, P., Wen, X., Xu, W., Li, Y., Jiang, C., Wu, Z., Zhang, H., & Liu, A. (2017). The siesta habit is associated with a decreased risk of rupture of intracranial aneurysms. Frontiers in Neurology, 8.
https://pubmed.ncbi.nlm.nih.gov/28936194/ -
Yang, Y., Liu, W., Ji, X., Ma, C., Wang, X., Li, K., & Li, J. (2020). Extended afternoon naps are associated with hypertension in women but not in men. Heart & Lung, 49(1), 2–9.
https://pubmed.ncbi.nlm.nih.gov/31521340/ -
Qu, H., Wang, H., Deng, M., Wei, H., & Deng, H. (2014). Associations between longer habitual day napping and non-alcoholic fatty liver disease in an elderly Chinese population. PLoS One, 9(8), e105583.
https://pubmed.ncbi.nlm.nih.gov/25140521/ -
Yamada, T., Shojima, N., Yamauchi, T., & Kadowaki, T. (2016). J-curve relation between daytime nap duration and type 2 diabetes or metabolic syndrome: A dose-response meta-analysis. Scientific Reports, 6(1).
https://pubmed.ncbi.nlm.nih.gov/27909305/ -
Léger, D., Torres, M. J., Bayon, V., Hercberg, S., Galan, P., Chennaoui, M., & Andreeva, V. A. (2019). The association between physical and mental chronic conditions and napping. Scientific Reports, 9(1).
https://pubmed.ncbi.nlm.nih.gov/30741949/ -
National Institute for Occupational Safety and Health. (2020, March 31). Napping, an important fatigue countermeasure. Centers for Disease Control and Prevention., Retrieved July 20, 2022, from
https://www.cdc.gov/niosh/emres/longhourstraining/napping.html -
Schwab, R. J. (2022, May). Insomnia and excessive daytime sleepiness (EDS). Merck Manual Professional Version., Retrieved July 20, 2022, from
https://www.merckmanuals.com/professional/neurologic-disorders/sleep-and-wakefulness-disorders/insomnia-and-excessive-daytime-sleepiness-eds -
Irish, L. A., Kline, C. E., Gunn, H. E., Buysse, D. J., & Hall, M. H. (2015). The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Medicine Reviews, 22, 23–36.
https://pubmed.ncbi.nlm.nih.gov/25454674/