When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
When Should Kids Stop Napping?
- While all children are unique, many begin to outgrow regular naps around the age of 5.
- A child may be ready to stop napping if they consistently resist naps, sleep through the night, or struggle to fall asleep at their current bedtime.
- Parents should gradually reduce the frequency and duration of naps.
- There may be occasional days when a child still needs a nap.
Sleep is essential to the well-being of children. Not only does sleep support the overall health of the child, but it also affects a child’s mood and his or her ability to learn during the daytime. A lack of sleep can have long-term impacts on a child’s future academic performance and emotional health.
As infants and children grow, the amount of daily sleep they need decreases. These sleep needs are initially distributed between naps and nighttime sleep, but at what age should kids stop napping?
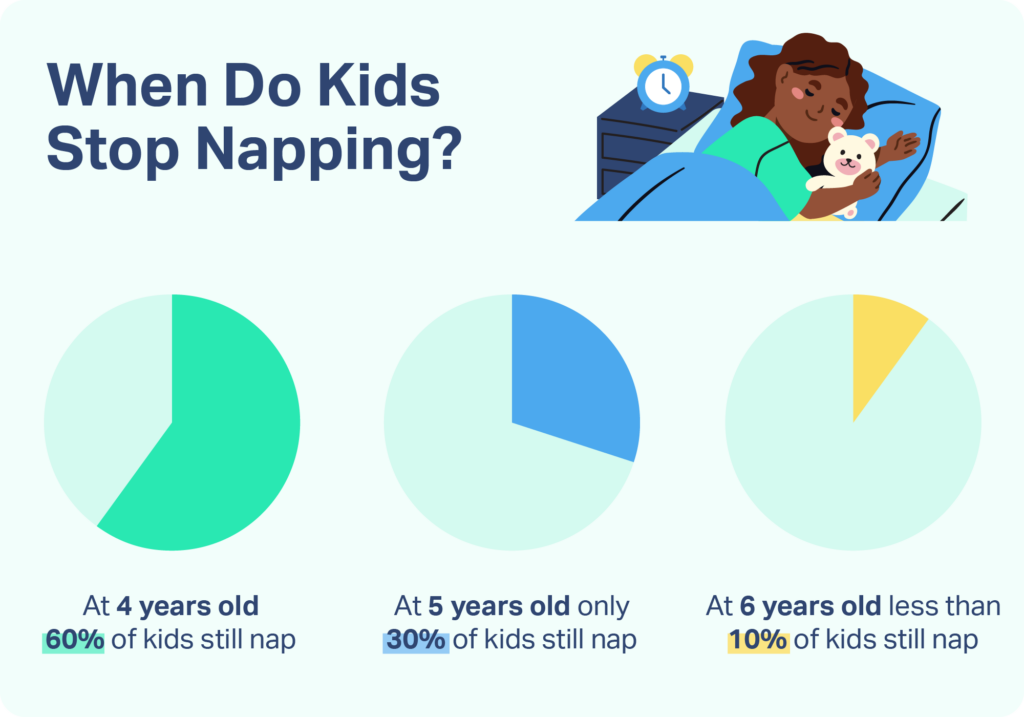
The exact age varies among children, depending on factors such as attending preschool, maturity, and nighttime sleep habits. At age three, almost all children still nap at least once per day. Sixty percent of four-year-olds still nap. However, by five years of age, most children no longer need naps, with less than 30% of children that age still taking them. The number decreases even more by age six, where less than 10% of children nap. Nearly all children stop napping by seven years of age. If your child is still napping regularly at age seven, consult your pediatrician to confirm there are no underlying sleep health concerns.
Help Your Child Sleep Better With Pediatric Sleep Coaching

our partner at sleepdoctor.com
Learn More“Life-changing! My anxiety about my son’s sleeping habits were immediately reduced after talking to Sara. She went above and beyond to tailor a schedule to our goals, answer our questions, keep us on track, and check in to encourage us when we just thought we couldn’t do it anymore.”
Rachael B. – Verified Customer
When Should Kids Stop Napping?
Because the age varies when children stop napping, it is important for parents to be attentive to their child’s needs. Generally speaking, kids should stop napping when they no longer need a nap to feel energized for a full day. Many children will stop napping naturally. There are several signs that indicate a child is ready to stop taking naps:
- They have difficulty falling asleep at nap time. Children who are no longer tired during the day — and who have a consistent mood during days without naps — may struggle to fall asleep when it is nap time. For instance, children may play or sing while laying in bed, or may simply not fall asleep. If a child is fussy during this time, it may indicate they still need to nap, but the timing of when the nap occurs may need to be adjusted.
- They have difficulty falling asleep at night time. Napping during the day can delay your child’s ability to fall asleep, leaving them with less sleep overall. The length of nap time can be reduced to help children become sleepy by bedtime. Avoid pushing your child’s bedtime later. Instead, monitor when the child is sleepy and put them down for bed at that time. In general, it is more advisable to shorten naps than push bedtimes later.
- They are waking up early. Daytime napping when it is no longer needed may cause your child to be fully rested well before their morning wake-up time. If your child still needs to nap but is waking early, try shortening their naps rather than eliminating the nap entirely.
- They don’t show signs of sleepiness on days without naps. If your child is not yawning or struggling to stay awake during the daytime, and she is not becoming cranky in the evening, she may be ready to stop taking naps.
- They are no longer napping at all. During their scheduled nap time, they may continue to play or read without signs of sleepiness.
When Do Kids Still Need Naps?
Infants until one year of age will take naps 1–4 times per day. As the brain matures, fewer and fewer naps are required. By 18-24 months, children need only one nap each day. Children who take early afternoon naps for a set duration of fewer than 60 minutes have been observed sleeping well at night. However, naps should not be shortened if the child is sleeping well at bedtime.
There are a few clear signs that your child is not ready to stop napping. Kids whose behaviors shift negatively in the evenings—such as becoming more irritable or overtired—are probably not ready to stop napping. A lack of sleep can negatively affect their emotions . If your child is struggling to stay awake during the daytime after a full night of sleep, they likely still need a daily nap. You might decrease the length of the nap to help them prepare for transitioning out of naptime habits.
How to Transition Kids Away From Naps
Transitioning away from naps may take time. Rather than quitting naps altogether, replacing nap time with quiet time can allow children to choose whether they’d like to sleep or play quietly. Many daycares and preschools offer this quiet time for children.
Just like nap time, quiet time should be structured in a specific location and set for a specific period of time. If they are not napping, children should have a stimulating activity so that they will sleep at night. Offer your child the choice of quiet activities such as reading, putting together a puzzle, or coloring. Whether sleeping or not, a period of rest can help with memory consolidation and recharging for the rest of the day.
Avoid replacing nap time with activities that induce drowsiness, such as driving or watching TV. Parents should also avoid loud activities themselves to encourage the child to play quietly. Loud noises may cause the child to leave their quiet time space.
How Sleep Changes Without Naps
When children no longer take naps, they may need more sleep at nighttime. It is recommended that parents make bedtime earlier for children who are no longer napping so that they have the necessary amount of sleep. Because preschool-aged children need up to 13 hours of sleep, bedtime may need to be moved up to 6 p.m. or 6:30 p.m., depending on what time your child needs to wake up.
To encourage sleep, it is recommended parents build a regular bedtime routine for their children. A nighttime routine can include a snack, hygiene such as brushing teeth or taking a bath, and reading or singing lullabies.
Occasional naps may still happen after children no longer have scheduled naptime. Growth spurts, changes in routine, and school may affect your child’s sleepiness. The return to naps is usually not a problem so long as the nap time is structured and does not affect the child’s nighttime sleep.
Keep in mind that as your child grows older, quiet time is still an important element of children’s lives. Also, be aware that napping in adolescents has been shown to be related to a decrease in nighttime sleep and sleep overall. Consult your pediatrician if you have concerns about your child’s sleep habits, or if there are any serious, sudden changes in your child sleeping too much or not enough.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
10 Sources
-
Consensus Conference Panel, Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., Dinges, D. F., Gangwisch, J., Grandner, M. A., Kushida, C., Malhotra, R. K., Martin, J. L., Patel, S. R., Quan, S. F., Tasali, E., Non-Participating Observers, Twery, M., Croft, J. B., Maher, E., … Heald, J. L. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Journal of Clinical Sleep Medicine, 11(6), 591–592.
https://pubmed.ncbi.nlm.nih.gov/25979105/ -
Weissbluth, M. (1995). Naps in Children: 6 Months– 7 Years. Sleep, 18(2), 82–87.
https://academic.oup.com/sleep/article-lookup/doi/10.1093/sleep/18.2.82 -
Akacem, L. D., Simpkin, C. T., Carskadon, M. A., Wright, K. P., Jr, Jenni, O. G., Achermann, P., & LeBourgeois, M. K. (2015). The Timing of the Circadian Clock and Sleep Differ between Napping and Non-Napping Toddlers. PloS one, 10(4), e0125181.
https://pubmed.ncbi.nlm.nih.gov/25915066/ -
Horváth, K., & Plunkett, K. (2018). Spotlight on daytime napping during early childhood. Nature and science of sleep, 10, 97–104.
https://pubmed.ncbi.nlm.nih.gov/29576733/ -
Nakagawa, M., Ohta, H., Nagaoki, Y., Shimabukuro, R., Asaka, Y., Takahashi, N., Nakazawa, T., Kaneshi, Y., Morioka, K., Oishi, Y., Azami, Y., Ikeuchi, M., Takahashi, M., Hirata, M., Ozawa, M., Cho, K., Kusakawa, I., & Yoda, H. (2016). Daytime nap controls toddlers’ nighttime sleep. Scientific reports, 6, 27246.
https://pubmed.ncbi.nlm.nih.gov/27277329/ -
Berger, R. H., Miller, A. L., Seifer, R., Cares, S. R., & LeBourgeois, M. K. (2012). Acute sleep restriction effects on emotion responses in 30- to 36-month-old children. Journal of sleep research, 21(3), 235–246.
https://pubmed.ncbi.nlm.nih.gov/21988087/ -
Tambini, A., Ketz, N., & Davachi, L. (2010). Enhanced brain correlations during rest are related to memory for recent experiences. Neuron, 65(2), 280–290.
https://pubmed.ncbi.nlm.nih.gov/20152133/ -
Lam, J. C., Mahone, E. M., Mason, T., & Scharf, S. M. (2011). The effects of napping on cognitive function in preschoolers. Journal of developmental and behavioral pediatrics : JDBP, 32(2), 90–97.
https://pubmed.ncbi.nlm.nih.gov/21217402/ -
Mindell, J. A., & Williamson, A. A. (2018). Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Medicine Reviews, 40, 93–108.
https://pubmed.ncbi.nlm.nih.gov/29195725/ -
Jakubowski, K. P., Hall, M. H., Lee, L., & Matthews, K. A. (2017). Temporal Relationships Between Napping and Nocturnal Sleep in Healthy Adolescents. Behavioral sleep medicine, 15(4), 257–269.
https://pubmed.ncbi.nlm.nih.gov/27078714/




















