When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
How Much Deep Sleep Do You Need?
At a Glance
Adults typically spend 10% to 20% of the night in deep sleep, also known as slow-wave sleep. That equals roughly 40 to 110 minutes of deep sleep for those who get the recommended seven to nine hours of total sleep.
Not all sleep is created equal—and when it comes to feeling truly rested, deep sleep does the heavy lifting. This essential stage plays a key role in everything from muscle recovery to immune health to brain function. Without enough of it, even a full night’s sleep can leave you feeling groggy and unrefreshed.
We take a closer look at this sleep stage, including what makes deep sleep unique, how much deep sleep you need, and how to make sure you’re getting the right amount of deep sleep.
What Is Deep Sleep?
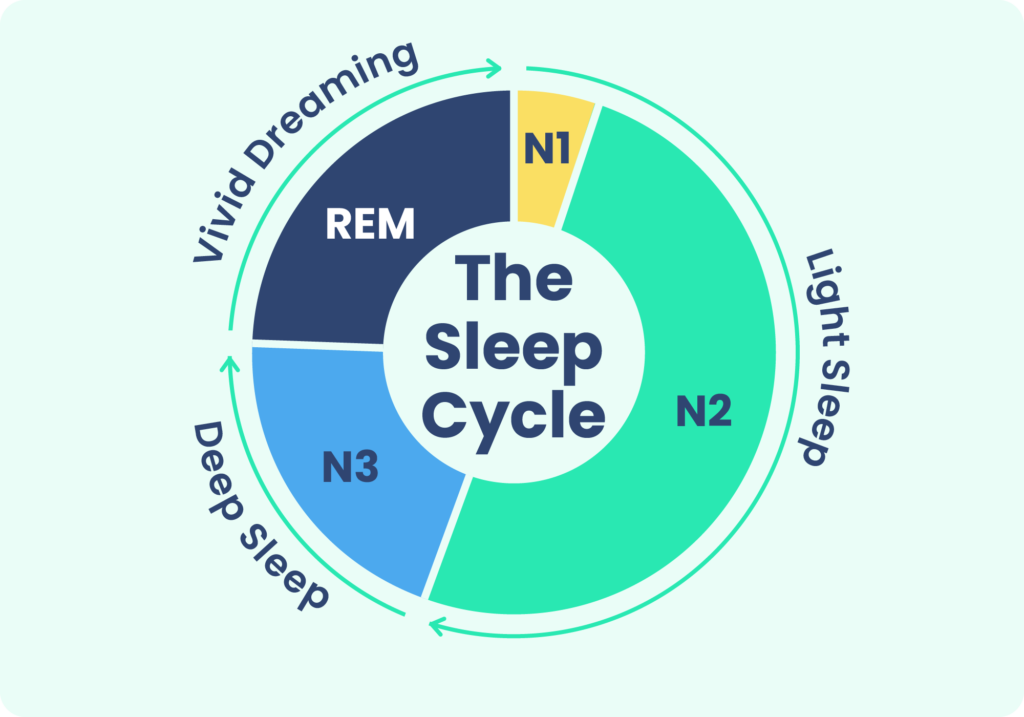
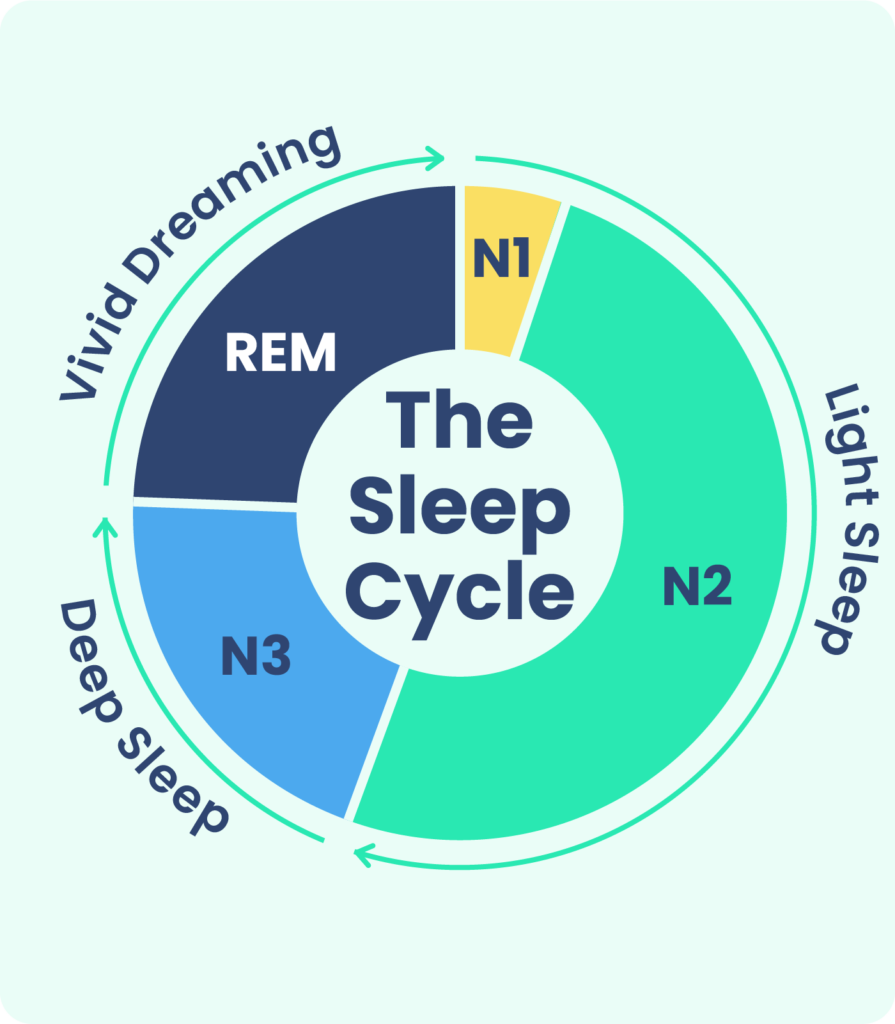
Deep sleep is a specific stage of sleep. When we sleep, we move through multiple sleep cycles that last 90 to 120 minutes and are made up of four different stages . A typical night involves four or five sleep cycles .
During deep sleep, your brain waves slow down, which is why deep sleep is also called slow-wave sleep . At the same time, deep sleep brings significant relaxation to your muscles and a pronounced slowing of your pulse and breathing rate .
When you’re in the deep-sleep stage, it can be hard for someone to wake you up. If you do get awakened from deep sleep, you may experience a fogginess that can last up to an hour. That groggy feeling is called sleep inertia.
Other Stages of Sleep
The four stages of sleep are separated into two categories: rapid eye movement (REM) sleep and non-REM (NREM) sleep. The first three stages, including deep sleep, are all stages of non-rapid eye movement sleep.
- Stage 1: This brief stage is when your drowsiness gives way to falling asleep. Your heartbeat and breathing start to slow down, but it’s still pretty easy to wake you up during this stage.
- Stage 2: In this stage of light sleep, your breathing and heart rate slow even more. Your temperature drops, and your muscles relax.
- Stage 3: Stage 3 sleep is deep sleep, which shows the greatest degree of relaxation in the body, as well as a specific pattern of slow brain waves. In this stage, your breathing and pulse are slow and steady.
- Stage 4 (REM): During REM sleep, your brain gets more active, almost as if you were awake, but your muscles don’t move. Your pulse and respiration speed up and become more erratic, and your eyes move quickly behind your eyelids. Dreams are most vivid during the REM stage.
It may be tempting to think that deep sleep and REM sleep are more important than other stages. While REM and deep sleep do have a profound impact on your health, all of the sleep stages are essential. Each stage has a role to play in your sleep cycles, and you need all of the stages for healthy sleep.
How Much Deep Sleep Is Enough?
During a healthy night’s sleep for most adults, deep sleep makes up between 10% and 20% of total sleeping time .
That said, there’s no consensus on a single, concrete number for how much deep sleep is normal or ideal. In fact, unless you’re spending the night in a sleep lab, it’s hard to know for sure exactly how much time you spend in each sleep stage.
Without knowing an exact time, it may help to instead focus on how you feel in the morning and throughout the day. Since deep sleep is essential to restful sleep, feeling refreshed and alert is a sign that you’re likely getting a good amount of deep sleep .
If you want to try to get more specific, the next few sections walk through how you can try to determine the amount of deep sleep that’s appropriate for you.
Total Sleep Time
To figure out how much deep sleep you need, first calculate how much sleep you need overall. Most adults should aim for at least seven hours of sleep each night.
If you’re not sure about how much sleep you really need, consider talking with your doctor for a recommendation based on your age and overall health.
Deep Sleep
Once you have a number for your total sleep time, calculate 10% and 20% of that number to determine the low- and high-end figures for how much deep sleep you’re aiming for.
For example, if your total sleep time is seven hours, your range for deep sleep would be between 42 and 84 minutes. If your total sleep time is eight hours, your range would be between 48 and 96 minutes.
REM Sleep
REM sleep typically makes up 20% to 25% of your nightly sleep. For most adults, that usually means up to two hours per night .
Factors Impacting Deep Sleep Needs
To a certain extent, deep sleep is self-regulating — when you haven’t gotten enough, your brain and body may seek it out the next time you sleep . For example, you might spend more time in deep sleep if you’re recovering from a period of sleep deprivation.
However, deep sleep needs can vary from person to person. Children and adolescents require the most deep sleep. Then, deep sleep starts to decrease over time and into older age .
There’s limited research about whether certain other groups of people need more deep sleep. Some studies have found that women spend proportionally more of their sleep time in deep sleep than men and have more intense deep sleep after being sleep deprived . However, it isn’t clear if women necessarily need more deep sleep.
Athletes who are involved in training activities frequently spend more of the night in deep sleep . This suggests that they may need more deep sleep for recovery, but more research is needed to fully understand the individual variability of deep sleep needs.
Track Your Sleep Quantity and Quality
Once you’ve calculated how much deep sleep you should be getting, it’s important to regularly assess whether your sleep is actually meeting your needs. One of the simplest ways to do this is by checking in with how you feel when you wake up. Do you feel well-rested and alert, or groggy and sluggish?
Sleep trackers can offer helpful insights by showing how much deep sleep you’re getting each night and how consistently you’re reaching your goals. According to a SleepFoundation.org survey, people who use a sleep tracker are more than two and a half times more likely than those who don’t to say they wake up feeling “very alert.” On the other hand, those who don’t use a tracker were almost 29% more likely to report feeling groggy in the morning.
While trackers aren’t perfect, they can highlight trends that point to whether you’re consistently getting enough deep, restorative sleep. Pair those insights with your own observations to determine if your sleep habits are working, and if not, consider making changes to improve both sleep quality and quantity.
Why Is Deep Sleep Important?
While all stages of sleep are necessary for good health, deep sleep offers specific physical and mental benefits. During deep sleep, your body works to build and repair tissue, muscles, and bones, including by producing high levels of growth hormone .
Deep sleep also promotes immune system functioning. Research suggests that it helps you build stronger immune responses and reduce unwanted chronic inflammation .
Slow-wave sleep also helps regulate blood sugar levels. As a result, the risk of developing type 2 diabetes may be higher if you don’t get enough deep sleep . And a shortage of deep sleep has also been linked to high blood pressure .
Deep sleep is important for cognitive function and memory. Although brain activity slows during deep sleep, this may actually facilitate learning by keeping the brain from becoming oversaturated with information. Evidence suggests that deep sleep also helps eliminate waste material from the brain, which may help protect against dementia .
Who Doesn’t Get Enough Deep Sleep?
Unfortunately, many people struggle to get enough deep sleep. Nearly a third of adults in the United States get less than the recommended amount of sleep , which also means reducing time for deep sleep.
People who have fragmented, low-quality sleep may also struggle to get all the deep sleep they need. A number of other factors can affect who doesn’t get enough deep sleep:
- Aging: Reduced deep sleep is a normal part of aging, with a gradual decline that levels off in your 70s.
- Insomnia: People with insomnia struggle with a lack of sleep quantity or quality, which can erode time spent in deep sleep.
- Sleep apnea:Obstructive sleep apnea causes many micro-awakenings during the night that make it challenging to get consistent amounts of deep sleep .
- Mental health conditions:Anxiety, depression, bipolar disorder, and schizophrenia are among the mental health conditions that can disrupt both deep sleep and REM sleep.
- Stress: Having high levels of stress, including from your work or personal life, may make it harder to get deep sleep.
- Dementia: Cognitive impairment, including dementia and Alzheimer’s disease, is associated with sleep disturbances that can reduce sleep quality and deep sleep .
- Pain: Dealing with pain at night can lead to sleep disruptions that throw off sleep cycles and reduce deep sleep. Arthritis, traumatic brain injury (TBI), and back pain are just a few examples of conditions that can cause pain and hinder deep sleep .
- Heart disease: Research has found that having heart disease is linked to reduced levels of deep sleep .
- Asthma: Conditions like asthma that disrupt breathing may fragment your sleep and negatively impact deep sleep.
- Pregnancy: Studies have found that deep sleep decreases during pregnancy but usually rebounds within a few months after giving birth .
- Certain drugs and medications: Various drugs and medications can alter sleep patterns and impact deep sleep. Examples include caffeine, alcohol, opioids, and some prescription drugs .
What Happens When You Don’t Get Enough Deep Sleep?
Because deep sleep is an essential component of your nightly rest, a shortage of deep sleep contributes to broader impacts of sleep deprivation. In addition to causing tiredness, a shortage of deep sleep can cause general symptoms of sleep deprivation, including :
- Reduced alertness and attention
- Trouble learning and remembering things
- Irritability
- Symptoms of depression or anxiety
- Increased likelihood of accidents and injuries
On top of these immediate effects, a chronic lack of quality sleep can increase the likelihood of multiple health problems, such as:
- Infections and reduced immune system function
- Obesity
- Type 2 diabetes
- Cardiovascular problems, including high blood pressure, stroke, and heart disease
- Kidney disease
Sleep Disorders Associated With Deep Sleep
The sleep disorders most associated with deep sleep are abnormal behaviors that occur when a person is partly awake and partly asleep. These are known as disorders of arousal or NREM parasomnias, and they usually arise while a person is in deep sleep .
When disorders of arousal occur, a person is not conscious of their behavior, and they don’t remember it afterward. The main types of disorders of arousal include :
- Sleepwalking: This involves getting out of bed and walking, running, jumping, or doing other activities like cleaning or preparing food.
- Confusional arousals: These episodes involve confusion and unclear speech or movements, but the person typically doesn’t leave the bed. Confusional arousals can include sexual behavior, which is sometimes called sexsomnia.
- Sleep terrors: During a sleep terror, a person appears to wake up with extreme fear. They may scream or yell and have a rapid pulse or heartbeat, but they aren’t consciously awake.
Disorders of arousal can affect people of any age, but they are more common in children. Getting insufficient sleep or having fragmented sleep can increase the risk of experiencing disorders of arousal.
How Can You Get More Deep Sleep?
If you want to get more deep sleep, focus on enhancing your overall sleep. If your sleep quality and quantity are good, it usually means you’re getting plenty of restorative deep sleep. You get the most deep sleep during the early part of the night.
One of the most reliable ways to improve your sleep is by practicing good sleep hygiene. Good habits include :
- Establishing a consistent bedtime and wake-up time
- Ensuring you have a quiet, cool, and dark sleep environment
- Creating a relaxing bedtime routine to wind down in the evening
- Reducing caffeine intake in the afternoon and evening
- Limiting use of mobile devices, tablets, laptops, and other screens for 30 minutes or more before bedtime
There are some additional steps you can try to encourage more deep sleep:
- Take a warm bath: Some research suggests that heating your body with a warm bath before bedtime may induce more slow-wave sleep . A warm bath raises body temperature, which promotes blood circulation, and the subsequent cooling may help ease the transition to sleep.
- Change your diet: What you eat and drink before bedtime impacts your sleep. One small study found that people eating a diet high in saturated fats obtained less slow-wave sleep . People who ate more fiber were more likely to have increased amounts of deep sleep.
- Listen to binaural beats:Binaural beats are created by listening to two slightly different tones, one in each ear. The difference between the frequencies of those tones creates a perceived third tone, or binaural beat. Limited research suggests that listening to certain binaural beats may contribute to more stage 3 sleep .

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
29 Sources
-
Schwab, R. J. (2022, September). Overview of sleep. Merck Manual Consumer Version.
https://www.merckmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/overview-of-sleep -
Kirsch, D. (2023, July 25). Stages and architecture of normal sleep. UpToDate.
https://www.uptodate.com/contents/stages-and-architecture-of-normal-sleep -
Patel, A. K., Reddy, V., Shumway, K. R., Araujo, J. F. (2024, January 26). Physiology, sleep stages. StatPearls.
https://www.ncbi.nlm.nih.gov/books/NBK526132/ -
National Institute of Neurological Disorders and Strokes (NINDS). (2024, September 05). Brain basics: Understanding sleep.
https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep -
Bollu, P. C., & Gurung, P. (2019, November 5). Normal sleep, sleep physiology, and sleep deprivation. Medscape.
https://emedicine.medscape.com/article/1188226-overview#showall -
Libman, E., Fichten, C., Creti, L., Conrod, K., Tran, D. L., Grad, R., Jorgensen, M., Amsel, R., Rizzo, D., Baltzan, M., Pavilanis, A., & Bailes, S. (2016). Refreshing Sleep and Sleep Continuity Determine Perceived Sleep Quality. Sleep disorders, 2016, 7170610. https://doi.org/10.1155/2016/7170610
https://pubmed.ncbi.nlm.nih.gov/27413553/ -
Consensus Conference Panel, Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., Dinges, D. F., Gangwisch, J., Grandner, M. A., Kushida, C., Malhotra, R. K., Martin, J. L., Patel, S. R., Quan, S. F., Tasali, E., Non-Participating Observers, Twery, M., Croft, J. B., Maher, E., … Heald, J. L. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Journal of Clinical Sleep Medicine, 11(6), 591–592.
https://pubmed.ncbi.nlm.nih.gov/25979105/ -
Blumberg, M. S., Lesku, J. A., Libourel, P. A., Schmidt, M. H., & Rattenborg, N. C. (2020). What is REM sleep?. Current Biology, 30(1), R38–R49.
https://pubmed.ncbi.nlm.nih.gov/31910377/ -
Cirelli, C. (2024, May). Insufficient sleep: Definition, epidemiology, and adverse outcomes. In R. Benca & A. Eichler (Ed.). UpToDate.
https://www.uptodate.com/contents/insufficient-sleep-definition-epidemiology-and-adverse-outcomes -
National Heart, Lung, and Blood Institute. How Sleep Works – Sleep Phases and Stages | NHLBI, NIH. www.nhlbi.nih.gov. Published March 24, 2022.
https://www.nhlbi.nih.gov/health/sleep/stages-of-sleep -
Mong, J. A., Cusmano, D. M. (2016). Sex differences in sleep: Impact of biological sex and sex steroids. Philosophical Transactions of the Royal Society, 371(1688).
https://pubmed.ncbi.nlm.nih.gov/26833831/ -
Vlahoyiannis A, Aphamis G, Bogdanis GC, Sakkas GK, Andreou E, Giannaki CD. Deconstructing athletes’ sleep: A systematic review of the influence of age, sex, athletic expertise, sport type, and season on sleep characteristics. J Sport Health Sci. 2021;10(4):387-402. doi:10.1016/j.jshs.2020.03.006
https://pubmed.ncbi.nlm.nih.gov/32325024/ -
Dijk D. J. (2009). Regulation and functional correlates of slow wave sleep. Journal of Clinical Sleep Medicine, 5(2 Suppl), S6–S15.
https://pubmed.ncbi.nlm.nih.gov/19998869/ -
Besedovsky, L., Lange, T., & Born, J. (2012). Sleep and immune function. Pflügers Archiv: European Journal of Physiology, 463(1), 121–137.
https://pubmed.ncbi.nlm.nih.gov/22071480/ -
Javaheri, S., Zhao, Y. Y., Punjabi, N. M., Quan, S. F., Gottlieb, D. J., & Redline, S. (2018). Slow-wave sleep is associated with incident hypertension: The sleep heart health study. Sleep, 41(1), zsx179.
https://pubmed.ncbi.nlm.nih.gov/29087522/ -
Zhang, Y., & Gruber, R. (2019). Can slow-wave sleep enhancement improve memory? A review of current approaches and cognitive outcomes. The Yale Journal of Biology and Medicine, 92(1), 63–80.
https://pubmed.ncbi.nlm.nih.gov/30923474/ -
National Heart Lung and Blood Institute. (2011, January). Your guide to healthy sleep. January 2011.
https://www.nhlbi.nih.gov/health-topics/all-publications-and-resources/your-guide-healthy-sleep -
Neikrug, A. B., & Ancoli-Isreail, S. (2023, February 3). Sleep-wake disturbances and sleep disorders in patients with dementia. In C. A. Goldstein & R. Benca (Eds.). UpToDate.
https://www.uptodate.com/contents/sleep-wake-disturbances-and-sleep-disorders-in-patients-with-dementia -
Lim, M.M, & Baumann, C.R. (2023, February 15). Sleep-wake disorders in patients with traumatic brain injury. In A. F. Eichler (Ed.). UpToDate.
https://www.uptodate.com/contents/sleep-wake-disorders-in-patients-with-traumatic-brain-injury -
A.D.A.M. Medical Encyclopedia. (2020, August 13). Sleep and your health. MedlinePlus.
https://medlineplus.gov/ency/patientinstructions/000871.htm -
Lee, K. A., Zaffke, M. E., & McEnany, G. (2000). Parity and sleep patterns during and after pregnancy. Obstetrics and gynecology, 95(1), 14–18.
http://linkinghub.elsevier.com/retrieve/pii/S002978449900486X -
Roehrs, T., Roth, T. (2022, April 13). The effects of medications on sleep quality and sleep architecture. In R. Benca (Ed.). UpToDate.
https://www.uptodate.com/contents/the-effects-of-medications-on-sleep-quality-and-sleep-architecture -
MedlinePlus: National Library of Medicine (US). (n.d.). Healthy Sleep.
https://medlineplus.gov/healthysleep.html -
Foldvary-Schaefer, N. (2023, September 7). Disorders of arousal from non-rapid eye movement sleep in adults. UpToDate.
https://www.uptodate.com/contents/disorders-of-arousal-from-non-rapid-eye-movement-sleep-in-adults -
Mainieri, G., Loddo, G., & Provini, F. (2021). Disorders of arousal: A chronobiological perspective. Clocks & Sleep, 3(1), 53–65.
https://pubmed.ncbi.nlm.nih.gov/33494408/ -
A.D.A.M. Medical Encyclopedia.(2022, May 12). Changing your sleep habits. MedlinePlus.
https://medlineplus.gov/ency/patientinstructions/000757.htm -
Maeda T, Koga H, Nonaka T, Higuchi S. Effects of bathing-induced changes in body temperature on sleep. J Physiol Anthropol. 2023;42(1):20. Published 2023 Sep 8. doi:10.1186/s40101-023-00337-0
https://pubmed.ncbi.nlm.nih.gov/37684642/ -
St-Onge, M. P., Roberts, A., Shechter, A., & Choudhury, A. R. (2016). Fiber and saturated fat are associated with sleep arousals and slow wave sleep. Journal of Clinical Sleep Medicine, 12(01), 19–24.
https://pubmed.ncbi.nlm.nih.gov/26156950/ -
Lee, M., Song, C. B., Shin, G. H., & Lee, S. W. (2019). Possible effect of binaural beat combined with autonomous sensory meridian response for inducing sleep. Frontiers in Human Neuroscience, 13, 425.
https://pubmed.ncbi.nlm.nih.gov/31849629/










