When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
4-Month Sleep Regression
- What is the 4-month sleep regression? The 4-month sleep regression is a developmental phase when babies who were sleeping well may suddenly start waking up more often and have trouble settling back to sleep.
- What causes the 4-month sleep regression? Neurological development changes how your baby cycles through sleep, transitioning from newborn patterns to more mature sleep stages.
- What are signs of the 4-month sleep regression? Common signs of sleep regression include more frequent night wakings, shorter naps, difficulty falling asleep, increased fussiness, and changes in appetite or mood during the day.
- What can caregivers do about the 4-month sleep regression? Caregivers can help maintain a consistent sleep routine, offer soothing reassurance, encourage independent sleep habits, and be patient as the baby adjusts.
Babies experience a lot of changes in their sleep pattern as they grow. Newborns start out sleeping in short segments, then over the course of a few months, they begin sleeping longer and spending more time sleeping at night. But sleep patterns can change quickly and can even seem to go in reverse at times. This is called a sleep regression, and though the timing varies, it’s not uncommon for one to occur at around 4 months (as well as 6, 8 , 12, and 18 months).
Knowing the causes, signs, and ways to cope with a 4-month sleep regression can help parents and caregivers develop healthy sleep habits and support their child’s sleep.
What Is the 4-Month Sleep Regression?
At around 4 months, a baby’s brain and body are developing rapidly , and the process of forming and linking different areas of the brain and nervous system may create instability in sleep , referred to as a sleep regression.
A newborn needs between 16 and 18 hours of sleep per day , which typically comes in one to three hour segments throughout the day.
This starts to change by around 3 to 4 months of age when a baby’s sleep starts to consolidate, meaning that they begin to sleep for longer periods at a time. While multiple naps are still the norm, they may have longer nighttime sleep sessions and sleep fewer total hours.
Do All Babies Have a 4-Month Sleep Regression?
Not all babies have a 4-month sleep regression. Research has shown that there’s a considerable amount of individual variation in infant sleep . Some babies may have no detectable sleep regression at 4 months, while others may have difficulty sleeping at this age or a few months earlier or later.
What Causes a 4-Month Sleep Regression?
A 4-month sleep regression can occur because babies are in the midst of a major transition away from a newborn sleep pattern. That transition isn’t always smooth and may have plateaus or setbacks like sleep regressions. There is typically no single cause for a 4-month sleep regression, but some contributing factors may include:
- Separation anxiety
- A greater awareness of their surroundings, which can result in overstimulation
- An uneven transition into consolidated sleep
- Disturbances in the infant’s sleep environment
Help Your Baby Sleep Better With Pediatric Sleep Coaching

our partner at sleepdoctor.com
Learn More“Life-changing! My anxiety about my son’s sleeping habits were immediately reduced after talking to Sara. She went above and beyond to tailor a schedule to our goals, answer our questions, keep us on track, and check in to encourage us when we just thought we couldn’t do it anymore.”
Rachael B. – Verified Customer
What Are Signs of the 4-Month Sleep Regression?
At about 4 months old, some babies show signs of worsening sleep. Your baby may display some sleep-related symptoms that can indicate a sleep regression.
- Difficulty falling asleep: It may take longer for your infant to initially fall asleep. They may also appear restless around the time they normally settle down for bed.
- Frequent nighttime awakenings: After putting your infant to bed, they may wake up during the night more often. These nighttime awakenings may be accompanied by crying or fussiness.
- Irritability upon waking: Disrupted sleep during a 4-month sleep regression may cause irritability or crying when the infant wakes up.
- Reduced total sleep time: You may notice that your baby is sleeping less overall, both at night and during the day. It is also common for feeding schedules to be disrupted during a 4-month sleep regression due to this shift in sleeping patterns.
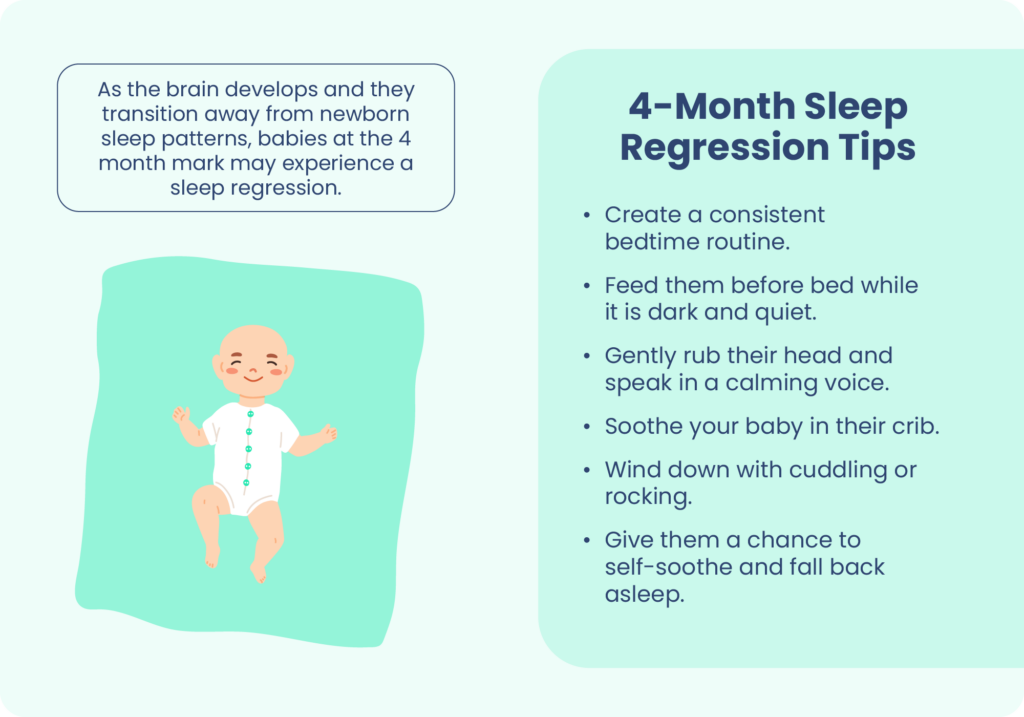
What Can Caregivers Do About the 4-Month Sleep Regression?
There’s no single solution to a 4-month sleep regression. Instead, caregivers are encouraged to cultivate healthy sleep routines and habits for their baby. These tips can help in the short-term and also create a framework for healthier sleep as your baby grows.
Adhere to Safe Sleep Guidelines
As you consider making changes to your baby’s sleep habits, make sure to review guidance for safe sleep and reducing the risk of sudden infant death syndrome (SIDS). Some risk reduction techniques for SIDS include removing soft items from the baby’s sleep space and putting the infant to bed on their back, according to the American Academy of Pediatrics (AAP).
Create a Sleep-Wake Routine
Establishing distinct routines during both waking and sleeping hours can help adjust your baby’s internal clock and encourage nighttime sleep. During the day, keep your baby active with playtime and provide access to natural light.
At night, allow your child to experience falling asleep in bed, as opposed to falling asleep somewhere else and then being put in bed. This can help them associate their bed with sleep and get them accustomed to falling asleep in bed on their own, which can help with self-soothing during nighttime awakenings. Feeding your baby shortly before bed can ensure they can stay asleep longer before their next feeding.
Your baby’s bedroom should be dark, quiet, and calm so that there are fewer sources of stimulation, distraction, or disturbance.
Help Your Baby Get Sleepy
Relaxing activities like cuddling or rocking can promote sleepiness. Try to identify signs like fussiness or eye rubbing that can indicate that your baby is tired. This can be a cue to start your bedtime routine so that you can put them in bed while drowsy.
Gently Encourage Your Baby Back to Sleep
If your infant wakes up during the night, it’s important to gently encourage a return to sleep. You may want to wait a minute before comforting them to see if they are able to self-soothe and fall back asleep. If you need to feed your baby during the night, try to do so as quickly as possible while keeping the room dark and quiet. As soon as they are fed, avoid playing with them or stimulating them and put them back to bed to return to sleep.
If your baby cries from separation anxiety when you put them in bed, resist the urge to pull them back out of their crib. Try being comforting and reassuring, lightly rubbing their head while talking in a soft, soothing voice until they calm down, at which point you can quietly walk away and let them fall asleep.
Self-Care for Caregivers
Self-care is an important part of parenting, and that includes recognizing that nighttime awakenings or sleep regressions are common in babies.
Caregivers should set realistic expectations and remember that it takes time for babies to develop stable sleep patterns. Many babies do not sleep through the night even at 12 months , so caregivers should avoid blaming themselves if their infant wakes up in the night. Self-care also includes considering tips to help parents get the sleep they need to feel more rested despite their baby’s sleep schedule.
When Should You Talk to Your Pediatrician?
Talk to your doctor if you have concerns about your baby’s sleep or increased nighttime awakenings. It is important to consult with your pediatrician if you also notice:
- Lack of growth or weight gain
- A reduced number of feedings
- Changes, especially reduction, in urination or bowel movements
Parents should also discuss any abnormal breathing during sleep with their pediatrician.
Frequently Asked Questions
How long does the 4-month sleep regression last?
In most cases, sleep problems only last for a few days to a few weeks, but this depends in part on fostering good sleep habits. Your baby’s sleep duration and quality may fluctuate over time as they continue to develop. Practicing good sleep hygiene with your infant can help resolve sleep regressions.
Is the 4-month sleep regression preventable?
Sleep regressions are a common and natural part of infant development and usually have no singular cause. Not all babies experience sleep regressions, while others may struggle with ongoing sleep issues throughout the first year of life. While a 4-month sleep regression may not be entirely preventable, establishing healthy sleep habits can improve your baby’s sleep overall.
Does the 4 month sleep regression affect naps?
Yes, the 4-month sleep regression often disrupts naps. Babies may start taking shorter naps, have trouble falling asleep during the day, or show signs of overtiredness due to more fragmented sleep.
What is a good bedtime for a 4-month-old?
A typical bedtime for a 4-month-old is between 6:30 p.m. and 8:00 p.m. Earlier bedtimes can help prevent over-tiredness and support longer nighttime sleep.
How much sleep does a 4-month-old need?
From the age of 4 to 12 months, it’s recommended that infants get 12 to 16 hours of sleep per day , including three to four daytime naps and around 10 to 12 hours of nighttime sleep, though it may still be broken into stretches.
How many times should a 4-month-old wake up at night?
It’s normal for a 4-month-old to wake one to three times per night for feeding or comfort. Some babies may wake more frequently during the regression as they adjust to new sleep cycles.
Can you sleep train during the 4-month sleep regression?
You can begin gentle sleep training during the 4-month sleep regression, but some sleep experts recommend waiting until 6 months of age. If you do attempt sleep training, it’s important to keep expectations realistic. Focus on establishing a consistent bedtime routine, offering comfort, and giving your baby brief opportunities to self-soothe.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
10 Sources
-
Testing Block Quote styles
-
Blumberg, M. S., Gall, A. J., & Todd, W. D. (2014). The development of sleep-wake rhythms and the search for elemental circuits in the infant brain. Behavioral neuroscience, 128(3), 250–263.
https://pubmed.ncbi.nlm.nih.gov/24708298/ -
Kirsch, D. (2022, September 12). Stages and architecture of normal sleep. In S. M. Harding (Ed.). UpToDate.
https://www.uptodate.com/contents/stages-and-architecture-of-normal-sleep -
A.D.A.M. Medical Encyclopedia. (2020, October 2). Bedtime habits for infants and children. MedlinePlus.
https://medlineplus.gov/ency/article/002392.htm -
Mindell, J. A., Leichman, E. S., Composto, J., Lee, C., Bhullar, B., & Walters, R. M. (2016). Development of infant and toddler sleep patterns: real-world data from a mobile application. Journal of sleep research, 25(5), 508–516.
https://onlinelibrary.wiley.com/doi/10.1111/jsr.12414 -
American Academy of Pediatrics (AAP). (2022 August 30). Getting your baby to sleep.
https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/Getting-Your-Baby-to-Sleep.aspx -
Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). (n.d.). Ways to Reduce The Risk Of SIDS And Other Sleep-Related Causes Of Infant Death.
https://safetosleep.nichd.nih.gov/safesleepbasics/risk/reduce -
Pennestri, M. H., Laganière, C., Bouvette-Turcot, A. A., Pokhvisneva, I., Steiner, M., Meaney, M. J., Gaudreau, H., & Mavan Research Team (2018). Uninterrupted Infant Sleep, Development, and Maternal Mood. Pediatrics, 142(6), e20174330.
https://publications.aap.org/pediatrics/article/142/6/e20174330/37494/Uninterrupted-Infant-Sleep-Development-and -
American Academy of Pediatrics (AAP). (2013, September 15). Sleeping Through the Night.
https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/Sleeping-Through-the-Night.aspx -
Paruthi, S., Brooks, L. J., D’Ambrosio, C., Hall, W. A., Kotagal, S., Lloyd, R. M., Malow, B. A., Maski, K., Nichols, C., Quan, S. F., Rosen, C. L., Troester, M. M., & Wise, M. S. (2016). Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: Methodology and discussion. Journal of Clinical Sleep Medicine, 12(11), 1549–1561.
https://pubmed.ncbi.nlm.nih.gov/27707447/





























