When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
6-Month Sleep Regression
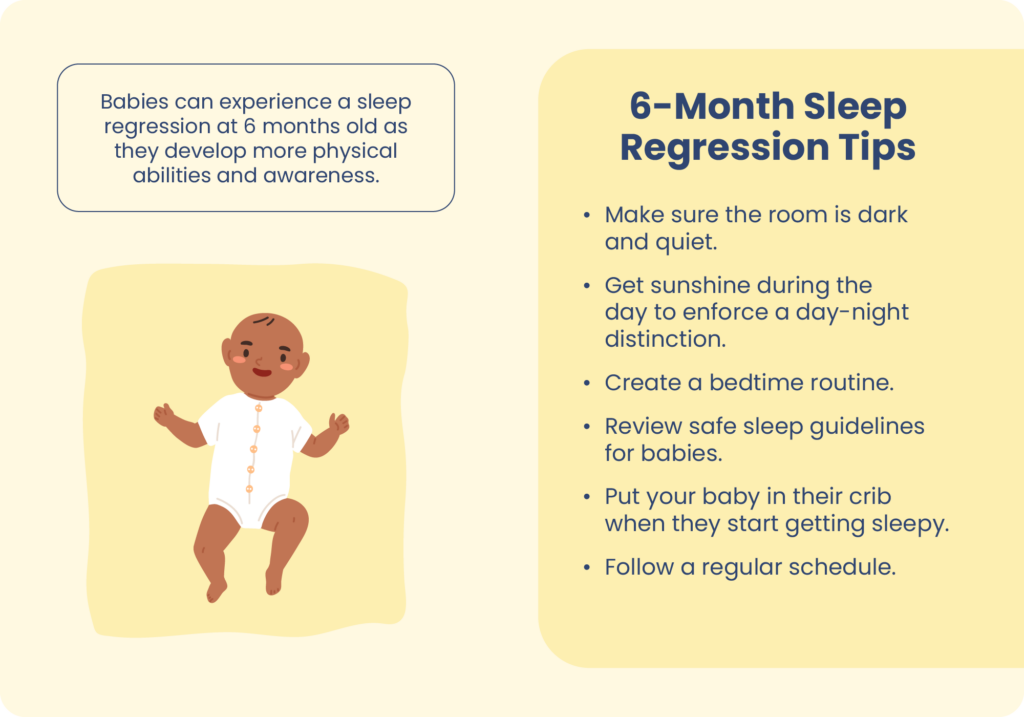
- Infants at 6 months of age become more aware of sounds and their environment, making them more sensitive to sleep disturbances.
- Signs of 6-month sleep regression include frequent wakings, difficulty falling asleep, longer naps during the day, and more crying at night.
- A 6-month sleep regression usually lasts for a few days or weeks.
- Reinforcing healthy sleep hygiene can help babies overcome sleep regression.
Between 4 and 6 months, many infants start to show noticeable progress toward sleeping for long periods and sleeping for much of the night. But sometimes that progress hits a snag, and sleeping difficulties can arise.
This is often called a sleep regression, and it represents a stop or a step backward in a baby’s progress toward consistent sleep. Although rarely long-lasting, a 6-month sleep regression can be a challenge for caregivers. Knowing the basics about infant sleep and strategies to improve it can help caregivers during a 6-month sleep regression and beyond.
How Does Infant Sleep Change Around 6 Months?
At 6 months of age, it is recommended that infants get between 12 and 16 total hours of sleep per day. Most babies of this age are starting to stay asleep for longer stretches at a time, a process known as sleep consolidation. Although they still usually nap a couple of times per day, a portion of their sleep shifts to nighttime, and many 6-month-olds start sleeping through the night .
Infants at 6 months are also undergoing significant physical and mental growth and typically reaching a number of developmental milestones . Awareness of their environment increases, they become more responsive to sounds, engage in more laughing and babbling, and they may gain physical abilities like rolling over or sitting unsupported. All of these factors may play a role in a baby’s activity level and sleep habits during the day and at night.
What Causes a 6-Month Sleep Regression?
In most cases, there is no single cause of a 6-month sleep regression. As babies grow, their development can unfold at an uneven pace, and this can result in periods when their sleep seems to hit a plateau or worsen.
Multiple factors can affect infant sleep. With an increase in their physical abilities and mental and environmental awareness, they may be more sensitive to overstimulation, separation anxiety, or other disturbances that can affect their sleep. With sleep consolidation, caregivers may be adjusting sleep schedules or routines, and it may take a baby time to acclimate to change.
Do All Babies Have a 6-Month Sleep Regression?
Some babies experience a 6-month sleep regression, but many do not. In fact, some caregivers may note a clear improvement in their baby’s sleep, including longer nighttime sleep periods, around this age.
While there are general patterns in infant sleep, research has found significant variability from one baby to the next . This means that it is normal for a child to have a sleep regression at 6 months or for their sleep to either stay the same or show signs of improvement at this age.
Help Your Baby Sleep Better With Pediatric Sleep Coaching

our partner at sleepdoctor.com
Learn More“Life-changing! My anxiety about my son’s sleeping habits were immediately reduced after talking to Sara. She went above and beyond to tailor a schedule to our goals, answer our questions, keep us on track, and check in to encourage us when we just thought we couldn’t do it anymore.”
Rachael B. – Verified Customer
What Are the Signs of a 6-Month Sleep Regression?
Potential signs of a 6-month sleep regression include:
- A greater number of awakenings at night that may involve more difficulty in getting back to sleep
- More problems falling asleep initially
- Longer naps during the day with less nighttime sleep
- More crying or agitation during awakenings
How long these symptoms occur can vary significantly. Usually, symptoms of a 6-month sleep regression last for short periods of time, especially if caregivers implement healthy sleep tips. Sleep problems often resolve within a few days or weeks, although a plateau in sleep improvements may continue for longer.
How Can Caregivers Manage Sleep Problems in 6-Month-Olds?
When a 6-month sleep regression occurs, it is an opportunity for caregivers to evaluate how they approach their child’s sleep. While there is no immediate fix for a sleep regression, following tips for healthy infant sleep can reinforce positive habits that promote better sleep in the short- and long-term .
Follow Safe Sleep Guidelines
It is important to review and continue to implement infant sleep safety measures , especially as a baby grows and can roll over on their own. Put infants to bed on their back and keep soft items out of their crib to reduce the risk of sudden infant death syndrome (SIDS).
Implement a Bedtime Routine
Use the same series of steps to get ready for bed each night as a way to signal to your infant that bedtime is approaching. Research has found this to improve infant sleep . Feed your baby before bed and engage in some calm activities, like rocking or cuddling, to help them wind down before sleep.
While you may not be able to manage a schedule to the minute, having a ritual with a regular time for bed and naps can create stability in your baby’s sleep pattern. Conversely, increased activity during the day, especially if it includes exposure to natural light, helps your baby get used to daytime being for play and nighttime being for sleep.
Facilitate Your Baby Falling Asleep in Bed
When your baby is showing signs of drowsiness, such as eye rubbing or fussiness, get them ready for bed and put them into their crib while sleepy but not yet asleep. This helps to associate their bed as a place to drift off to sleep.
Keep your child’s sleep area quiet and dark with as few potential disturbances as possible. If external noise carries into the child’s sleep space, a white noise machine may help.
Even if you follow all of these steps perfectly, your baby may still wake up during the night. If that happens, you may want to avoid rushing in immediately. Wait for a minute or two to see if your baby is able to calm down and get back to sleep on their own. If you do need to check on them, or if they need to be fed, keep light and sound to a minimum and do your best to avoid stimulation that could make it harder for them to fall asleep again.
Separation anxiety may cause your baby to cry when you walk away from their crib. If this occurs, resist the temptation to take them out of the crib. Instead, try techniques to gently comfort them such as rubbing their head or speaking in a quiet, calming voice. Once they have relaxed, you can move away from the crib and allow them to drift off to sleep.
When Should Caregivers Talk With a Doctor About Sleep Problems in 6-Month-Olds?
Sleeping problems in 6-month-olds do not usually require medical attention. However, you can always raise questions about a baby’s sleep during normal check-ins with their pediatrician.
It is best to check with your baby’s doctor about sleep regressions if you also notice other issues such as:
- Stunted growth or lack of weight gain
- Reductions in appetite or feeding
- Reductions in urination or bowel movements
- Labored or abnormal breathing
Self-Care For Caregivers
Caregivers of infants should remember the importance of self-care and getting the sleep they need. While it can be tempting to focus entirely on a baby’s needs, healthier caregivers are in a better position to provide loving and attentive care for their infant.Part of this self-care is avoiding self-blame when an infant has sleeping problems. It is common for babies to have trouble sleeping through the night even when they are a year old. Recognizing that a baby may go through phases of better or worse sleep can help caregivers set reasonable expectations and adapt to the way that their specific child grows and develops.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
11 Sources
-
Paruthi, S., Brooks, L. J., D’Ambrosio, C., Hall, W. A., Kotagal, S., Lloyd, R. M., Malow, B. A., Maski, K., Nichols, C., Quan, S. F., Rosen, C. L., Troester, M. M., & Wise, M. S. (2016). Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: Methodology and discussion. Journal of Clinical Sleep Medicine, 12(11), 1549–1561.
https://pubmed.ncbi.nlm.nih.gov/27707447/ -
Gradisar, M., Jackson, K., Spurrier, N. J., Gibson, J., Whitham, J., Williams, A. S., Dolby, R., & Kennaway, D. J. (2016). Behavioral interventions for infant sleep problems: A randomized controlled trial. Pediatrics, 137(6), e20151486.
https://pubmed.ncbi.nlm.nih.gov/27221288/ -
Camerota, M., Tully, K. P., Grimes, M., Gueron-Sela, N., & Propper, C. B. (2018). Assessment of infant sleep: How well do multiple methods compare? Sleep, 41(10), zsy146.
https://pubmed.ncbi.nlm.nih.gov/30085305/ -
National Center on Birth Defects and Developmental Disabilities (NCBDDD), Centers for Disease Control and Prevention (CDC). (2022, December 6). Important milestones: Your baby by six months., Retrieved April 25, 2023, from
https://www.cdc.gov/ncbddd/actearly/milestones/milestones-6mo.html -
Mindell, J. A., Leichman, E. S., Composto, J., Lee, C., Bhullar, B., & Walters, R. M. (2016). Development of infant and toddler sleep patterns: real-world data from a mobile application. Journal of sleep research, 25(5), 508–516.
https://onlinelibrary.wiley.com/doi/10.1111/jsr.12414 -
American Academy of Pediatrics (AAP). (2022, August 30). Getting Your Baby to Sleep., Retrieved April 25, 2023, from
https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/Getting-Your-Baby-to-Sleep.aspx -
A.D.A.M. Medical Encyclopedia. (2020, October 2). Bedtime habits for infants and children. MedlinePlus., Retrieved April 25, 2023, from
https://medlineplus.gov/ency/article/002392.htm -
Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). (n.d.). Ways to Reduce The Risk Of SIDS And Other Sleep-Related Causes Of Infant Death., Retrieved April 25, 2023, from
https://safetosleep.nichd.nih.gov/safesleepbasics/risk/reduce -
Mindell, J. A., Li, A. M., Sadeh, A., Kwon, R., & Goh, D. Y. (2015). Bedtime routines for young children: A dose-dependent association with sleep outcomes. Sleep, 38(5), 717–722.
https://pubmed.ncbi.nlm.nih.gov/25325483/ -
American Academy of Pediatrics (AAP). (2013, September 5). Sleeping through the night., Retrieved April 25, 2023, from
https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/Sleeping-Through-the-Night.aspx -
Pennestri, M. H., Laganière, C., Bouvette-Turcot, A. A., Pokhvisneva, I., Steiner, M., Meaney, M. J., Gaudreau, H., & Mavan Research Team (2018). Uninterrupted Infant Sleep, Development, and Maternal Mood. Pediatrics, 142(6), e20174330.
https://publications.aap.org/pediatrics/article/142/6/e20174330/37494/Uninterrupted-Infant-Sleep-Development-and





























