When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
How Much Sleep Do You Need?
- Most healthy adults need between seven and nine hours of sleep each night.
- Infants, young children, and teenagers should get more sleep to support their growth and development.
Feel like you’re constantly chasing sleep but never sure if you’re getting enough? Figuring out how much sleep you actually need can feel like solving a mystery. But sleep isn’t a luxury—it’s a biological necessity—and getting the right amount can mean the difference between powering through your day and dragging yourself through it.
So how many hours do you really need to feel rested, focused, and at your best? Let’s break it down.
How Many Hours of Sleep Do You Need?
As a basic rule, healthy adults need at least seven hours of sleep per night . Babies, young children, and teens need even more sleep to enable their growth and development .
Getting less than seven hours has been linked to a weakened immune system, reduced job performance, and a heightened risk of accidents (including car accidents). An ongoing lack of sleep is also associated with many serious health issues, including high blood pressure, heart disease, weight gain, obesity, diabetes, and depression.
If seven hours is the minimum, a natural follow-up question is whether adults can sleep too much. According to experts, the answer isn’t so clear. Sometimes sleeping more than nine hours is a sign of an underlying health problem, but getting extra sleep can be appropriate in certain circumstances, such as when you’re sick or trying to catch up on sleep.
Looking to improve your sleep? Try upgrading your mattress.
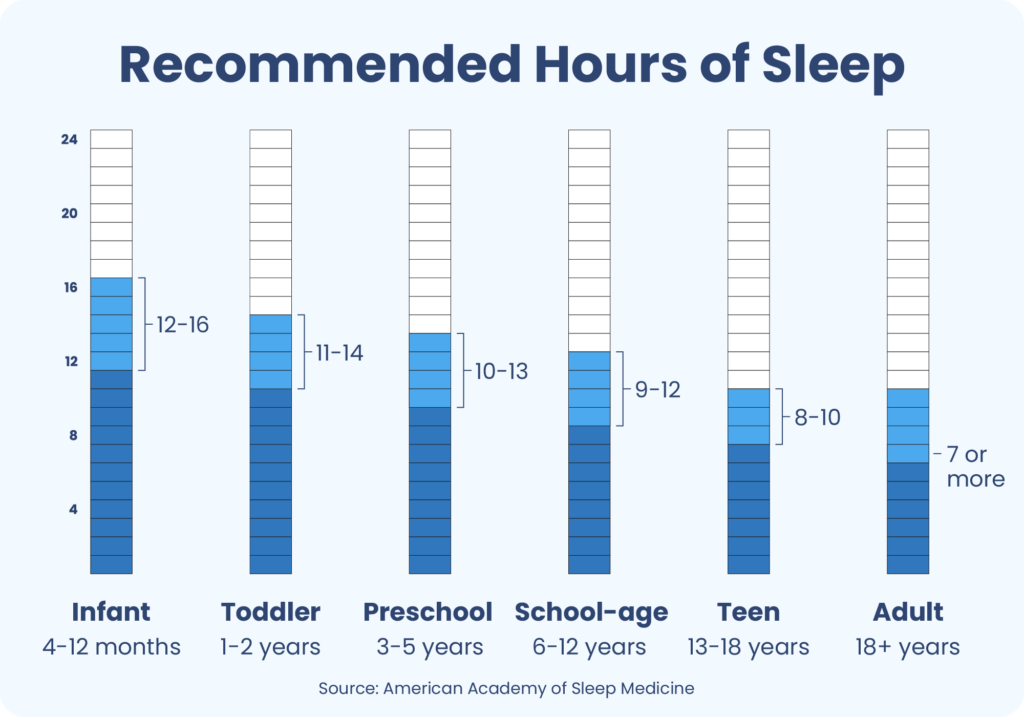
Recommended Hours of Sleep by Age
The amount of sleep a person needs depends on their age. Experts at organizations like the American Academy of Sleep Medicine, Sleep Research Society, and the American Academy of Pediatrics have endorsed a recommended sleep chart by age.
| Age group | Age range | Recommended hours of sleep |
|---|---|---|
| Infant | 4-12 months | 12-16 hours (including naps) |
| Toddler | 1-2 years | 11-14 hours (including naps) |
| Preschool | 3-5 years | 10-13 hours (including naps) |
| School-age | 6-12 years | 9-12 hours |
| Teen | 13-18 years | 8-10 hours |
| Adult | 18 years and older | 7 hours or more |
There’s no specific recommendation for newborns, because there’s limited research about how much sleep they truly need. That said, babies under four months often sleep between 14 and 17 hours per day .
Finding the Right Amount of Sleep for You
These guidelines serve as a rule of thumb for how much sleep babies, children, and adults need. Experts acknowledge that the ideal amount of sleep can vary from person to person . Some people need more or less sleep than the suggested amount for their age.
Deciding how much sleep you need means considering your overall health, daily activities, and typical sleeping patterns. Some questions that can help you assess your individual sleep needs include:
- Are you productive, healthy, and happy on seven hours of sleep? Or have you noticed that you require more hours of sleep to get into high gear?
- Do you unwillingly doze off during the day?
- Do you have health issues that might require more rest? Are you taking any medications that affect your sleep or daytime energy levels?
- Do you have a high level of daily energy expenditure? Do you frequently play sports or work in a labor-intensive job?
- Do your daily activities require alertness to do them safely? Do you drive every day or operate heavy machinery? Do you feel sleepy while doing these activities?
- Are you experiencing or do you have a history of a sleep disorder?
- Do you depend on caffeine to get you through the day?
- When you have an open schedule, do you tend to sleep more?
- Are you pregnant or breastfeeding?
You can use your answers to these questions to hone in on your optimal amount of sleep. You can also talk to your doctor to review your overall health, your typical sleep patterns, and whether you might need more or less sleep than recommended.
You may find that having sleep-related data can help you think about these questions. For example, keeping a sleep diary or wearing a sleep tracker may help you detect trends in how you sleep at night and how it affects you during the day.
Sleep Quality vs. Quantity
When thinking about sleep needs, it’s easy to focus on quantity. But a good night’s rest isn’t just about how many hours you’re asleep—the quality of your sleep is just as important.
Low-quality sleep often feels restless or disrupted, making it less refreshing than solid, continuous sleep . Fragmented sleep hinders your ability to progress through the four stages of sleep, all of which are necessary for healthy sleep .
Research is increasingly finding that poor quality sleep can be just as harmful as a reduced quantity of sleep . Disrupted sleep has been linked to many symptoms of sleep deprivation, including impaired memory and poor mood . Low-quality sleep may also raise long-term risks of numerous mental and physical health problems .
REM and Deep Sleep
Each night, we move through multiple sleep cycles that last 90 to 120 minutes . These sleep cycles are made up of four stages of sleep. All four stages are important to good sleep, but two specific stages have an especially big impact.
During deep sleep, also known as stage 3 sleep, your breathing and heart rate slow down, and your brain and body relax . This aids in your body’s rest and recovery, allowing you to wake up feeling rejuvenated.
Deep sleep also contributes to the health of your immune system, bones, and other tissues . On most nights, deep sleep makes up around 10% to 20% of your total sleep time, or about 90 minutes if you sleep for seven to eight hours .
Rapid eye movement (REM) sleep is the last sleep stage, and it usually makes up 20% to 25% of your time asleep (or about two hours) . During REM sleep, your pulse and breathing get faster, and brain activity picks up significantly, almost to the level of being awake . Dreaming is most active and intense during REM sleep. Research has found REM sleep is important for memory, mood, and overall brain function .
How Do You Know if You’re Getting Enough Sleep?
It’s challenging to know if you’re actually getting enough sleep. Reflecting on three key factors can help determine if you’re getting the right amount of rest.
- How you wake up: If you feel refreshed when you wake up, that’s a good sign. If you struggle to start your day, it may indicate that you’re short on sleep.
- Sleepiness during the day: If you find that you’re nodding off or extremely tired during the day, it could be a result of insufficient sleep at night.
- Your concentration levels: Good sleep helps you focus, so if you have trouble with concentration, it might be because you’re not getting enough sleep.
Track Your Sleep Quantity and Quality
Sleep tracking devices and apps can reveal patterns in your sleep duration, quality, and disruptions, giving you a clearer picture of whether your nightly rest is restorative.
According to a SleepFoundation.org survey, people who use a sleep tracker are more than two and a half times more likely than those who don’t to report waking up feeling “very alert.” Conversely, people who don’t use a tracker were nearly 20% more likely to say they wake up feeling groggy.
While sleep trackers can’t diagnose disorders, they can be a useful tool for developing better sleep habits. Use them in combination with a simple self-check each morning: Do you feel refreshed? Are you able to stay alert and focused throughout the day without relying heavily on caffeine? If not, you may not be getting enough quality sleep — even if your total time in bed seems sufficient.
What Happens if You Don’t Get Enough Sleep?
Not getting enough sleep can have far-reaching consequences. Some of the immediate signs of sleep deprivation include:
- Extreme tiredness during the day
- Slowed thinking and reaction time, heightening the risk of errors and accidents
- Reduced focus and memory
- Irritability
- Feelings of anxiety or depression
If insufficient sleep becomes a lasting problem, it can also give rise to other health issues, including:
- High blood pressure, heart problems, and stroke
- Decreased immune function
- Type 2 diabetes
- Kidney disease
- Obesity
How Can You Improve Your Sleep?
To improve your sleep, start by making sleep a priority in your schedule. This means calculating the hours you need so that work or social activities don’t infringe on time for sleep.
It’s also worth taking steps to boost your sleep quality. Enhancing your bedroom setting and sleep-related habits can make it easier to get the quantity and quality of sleep you need. Practical ways that you can improve your sleep hygiene include :
- Sticking to the same sleep schedule every day, even on weekends
- Practicing a relaxing bedtime routine to make it easier to fall asleep quickly
- Choosing a supportive, comfortable mattress and outfitting your bed with quality pillows and bedding
- Minimizing potential disruptions from light and sound while optimizing your bedroom temperature (between 65 and 68 degrees Fahrenheit)
- Disconnecting from electronic devices like mobile phones and laptops for at least 30 minutes and ideally an hour before bed
- Avoiding caffeine in the late afternoon or evening
- Limiting alcohol consumption, especially in the hours before bed
If you’re a parent or caregiver, many of the same tips apply to help children and teens get the recommended amount of sleep.If you or a family member are experiencing symptoms such as significant sleepiness during the day, insomnia, leg cramps, snoring, or another issue that is preventing you from sleeping well, talk with a doctor to determine the underlying cause.
Frequently Asked Questions
What is the 10-3-2-1-0 rule for sleep?
The 10-3-2-1-0 rule is a method of enhancing sleep hygiene. Each number represents a certain habit that can make it easier to get good sleep.
-Avoid caffeine consumption for 10 hours before bedtime.
-Do not drink alcohol or eat any food for 3 hours before going to bed.
-Finish all work-related tasks 2 hours before bed to give your mind time to wind down.
-Stop all screen time, including with your TV or phone, for 1 hour before bedtime.
-Wake up when your alarm goes off in the morning with 0 uses of the snooze button.
Why is it important to sleep between 10 p.m. and 2 a.m.?
Your body’s internal clock, also known as its circadian rhythm, functions best when it’s aligned with the timing of day and night
. So sleeping when it’s dark outside (between the hours of 10 p.m. and 2 a.m.) can support better alignment of your circadian rhythm
. It’s also when you tend to spend the most time in the deep sleep stage, so not sleeping during these hours may affect whether your sleep feels refreshing.
Ultimately, you may not always be able to sleep the entirety of the time between 10 p.m. and 2 a.m., but trying to coordinate your schedule to be sleeping when it’s dark outside can help limit circadian misalignment.
Why am I still tired after sleeping for 8 hours?
Unrefreshing sleep is frequently a consequence of restless sleep. For example, you might have been in bed for eight hours but spent part of that time tossing and turning. This is a common problem for people with insomnia or who have other health issues like acid reflux that interfere with sleep.
It could also be a sign of an underlying sleep disorder. Some sleep disorders cause repeated awakenings during the night that detract from your sleep quality, these awakenings are so brief that you don’t even realize they’re happening.
For example, sleep apnea, a condition involving repeated breathing interruptions during sleep, can make sleep unrefreshing regardless of how many hours you sleep. Other types of less-common sleep disorders also cause excessive daytime sleepiness
.
Is it healthy to nap during the day?
For adults, napping during the day can be healthy, but you want to nap strategically. That means considering the timing and length of any nap.
Nap timing: You don’t want to nap too late in the afternoon, which can make it harder for you to fall asleep at your normal bedtime
.
Nap length: To avoid waking up groggy from a nap, you should nap for either a maximum of 20 minutes or for about 90 minutes. In this way, you either wake up before entering deeper stages of sleep or you are able to complete a full sleep cycle before waking up.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of product specialists, sleep health professionals, and people just like you. Whether you’re searching for the perfect mattress or need expert sleep advice, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
22 Sources
-
Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med 2015;11(6):591–592.
https://jcsm.aasm.org/doi/10.5664/jcsm.4758 -
Paruthi, S., Brooks, L. J., D’Ambrosio, C., Hall, W. A., Kotagal, S., Lloyd, R. M., Malow, B. A., Maski, K., Nichols, C., Quan, S. F., Rosen, C. L., Troester, M. M., & Wise, M. S. (2016). Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: Methodology and discussion. Journal of Clinical Sleep Medicine, 12(11), 1549–1561.
https://pubmed.ncbi.nlm.nih.gov/27707447/ -
A.D.A.M. Medical Encyclopedia. (2020, October 2). Bedtime habits for infants and children. MedlinePlus.
https://medlineplus.gov/ency/article/002392.htm -
Cirelli, C. (2024, May). Insufficient sleep: Definition, epidemiology, and adverse outcomes. In R. Benca & A. Eichler (Ed.). UpToDate.
https://www.uptodate.com/contents/insufficient-sleep-definition-epidemiology-and-adverse-outcomes -
Libman, E., Fichten, C., Creti, L., Conrod, K., Tran, D. L., Grad, R., Jorgensen, M., Amsel, R., Rizzo, D., Baltzan, M., Pavilanis, A., & Bailes, S. (2016). Refreshing Sleep and Sleep Continuity Determine Perceived Sleep Quality. Sleep disorders, 2016, 7170610. https://doi.org/10.1155/2016/7170610
https://pubmed.ncbi.nlm.nih.gov/27413553/ -
MedlinePlus: National Library of Medicine (US). (n.d.). Healthy Sleep.
https://medlineplus.gov/healthysleep.html -
Van Someren, E. J., Cirelli, C., Dijk, D. J., Van Cauter, E., Schwartz, S., & Chee, M. W. (2015). Disrupted sleep: From molecules to cognition. The Journal of Neuroscience, 35(41), 13889–13895.
https://pubmed.ncbi.nlm.nih.gov/26468189/ -
Rolls, A., Colas, D., Adamantidis, A., Carter, M., Lanre-Amos, T., Heller, H. C., & de Lecea, L. (2011). Optogenetic disruption of sleep continuity impairs memory consolidation. Proceedings of the National Academy of Sciences of the United States of America, 108(32), 13305–13310.
https://pubmed.ncbi.nlm.nih.gov/21788501/ -
Finan, P. H., Quartana, P. J., & Smith, M. T. (2015). The effects of sleep continuity disruption on positive mood and sleep architecture in healthy adults. Sleep, 38(11), 1735–1742.
https://pubmed.ncbi.nlm.nih.gov/26085289/ -
Medic, G., Wille, M., & Hemels, M. E. (2017). Short- and long-term health consequences of sleep disruption. Nature and Science of Sleep, 9, 151–161.
https://pubmed.ncbi.nlm.nih.gov/28579842/ -
Schwab, R. J. (2022, September). Overview of sleep. Merck Manual Consumer Version.
https://www.merckmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/overview-of-sleep -
National Institute of Neurological Disorders and Strokes (NINDS). (2024, September 05). Brain basics: Understanding sleep.
https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep -
Patel, A. K., Reddy, V., Shumway, K. R., Araujo, J. F. (2024, January 26). Physiology, sleep stages. StatPearls.
https://www.ncbi.nlm.nih.gov/books/NBK526132/ -
Bollu, P. C., & Gurung, P. (2019, November 5). Normal sleep, sleep physiology, and sleep deprivation. Medscape.
https://emedicine.medscape.com/article/1188226-overview#showall -
Blumberg, M. S., Lesku, J. A., Libourel, P. A., Schmidt, M. H., & Rattenborg, N. C. (2020). What is REM sleep?. Current Biology, 30(1), R38–R49.
https://pubmed.ncbi.nlm.nih.gov/31910377/ -
What happens during sleep? Eunice Kennedy Shriver National Institute of Child Health and Human Development.
https://www.nichd.nih.gov/health/topics/sleep/conditioninfo/what-happens. -
Di T, Zhang L, Meng S, et al. The impact of REM sleep loss on human brain connectivity. Transl Psychiatry. 2024;14(1):270. Published 2024 Jul 2. doi:10.1038/s41398-024-02985-x
https://pubmed.ncbi.nlm.nih.gov/38956035/ -
A.D.A.M. Medical Encyclopedia.(2022, May 12). Changing your sleep habits. MedlinePlus.
https://medlineplus.gov/ency/patientinstructions/000757.htm -
National Heart, Lung, and Blood Institute. (2022, March). Circadian rhythm disorders: What are circadian rhythm disorders?
https://www.nhlbi.nih.gov/health/circadian-rhythm-disorders -
Schwab, R. J. (2022, May). Circadian rhythm sleep disorders. Merck Manual Professional Version.
https://www.merckmanuals.com/professional/neurologic-disorders/sleep-and-wakefulness-disorders/circadian-rhythm-sleep-disorders -
Preda, A. & Bowman, D. R. (2018, September 5). Primary hypersomnia workup. Medscape.
https://emedicine.medscape.com/article/291699-workup -
National Institute for Occupational Safety and Health. (2020, March 21). NIOSH training for nurses on shift work and long work hours. Centers for Disease Control and Prevention.
https://www.cdc.gov/niosh/work-hour-training-for-nurses/longhours/mod3/08.html