When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Can You Overdose on Melatonin?
- There’s no standard dosage of melatonin, but most adults should take between 1 to 5 milligrams and not exceed 10 milligrams a day.
- You should talk to a doctor before giving melatonin to children and not exceed doses of 3 milligrams for kids 5 and up. Kids under 5 should not take melatonin.
- In most cases, you can treat melatonin overdoses with time and rest. Very few require hospitalization.
- Life-threatenting overdoses are rare, but overdoses can cause noticeable side effects, including difficulty breathing, seizures, or a loss of consciousness.
Melatonin is one of the most popular sleep aids. In fact, in a recent Sleep Foundation survey, it topped the list of sleep aids, with 58% of respondents reporting they had previously used melatonin.
And though it’s been found generally safe with few serious side effects , there’s still a risk of melatonin overdose if you take too much. In recent years, poison centers have received five times the number of calls about melatonin overdose as they did 20 years ago. Emergency rooms have seen four times as many children and infants coming in after unintentional melatonin ingestion.
It’s important to be aware of the safety risks posed by taking too much melatonin. Below, we take a closer look at melatonin dosing, potential symptoms of a melatonin overdose, and when to contact a doctor.
How Much Melatonin Is Too Much?
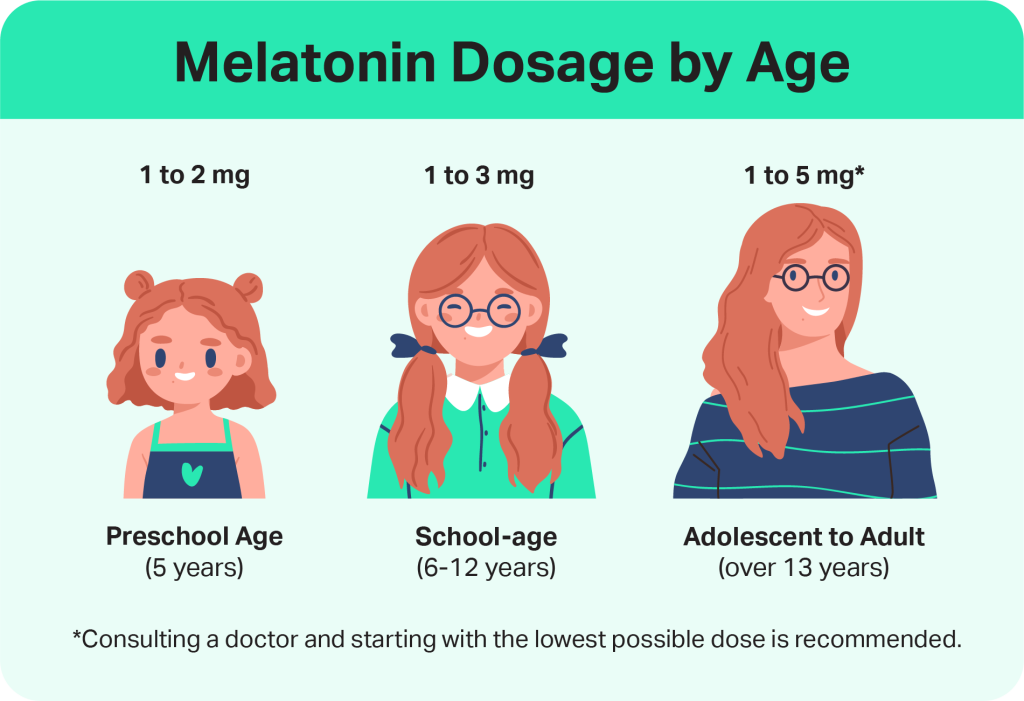
Recommended melatonin dosage varies depending on a person’s age. Experts generally recommend adults take between 1 and 5 milligrams of melatonin to promote better sleep.
Most adults shouldn’t need to take more than 5 milligrams of melatonin a day, and researchers have found that more than 10 milligrams of melatonin a day is too much .
It’s important to talk to your doctor before beginning melatonin supplementation. Start with a low dose of melatonin to see how your body reacts, then gradually increase the dosage if needed. Small doses, such as 1 milligram or less, may be just as effective as higher doses.
Starting with a low dose is especially important, because some melatonin supplements contain a higher dose than what’s listed on the label.
In the U.S., dietary supplements including melatonin aren’t tested by the Food and Drug Administration (FDA) for safety or accuracy prior to being sold, so the listed amount may be slightly or significantly different from what’s actually present in the supplement. Some supplements may also include more than just melatonin.
It’s also important to note that different formulations of melatonin, such as pill, powder, gummy, or liquid, may be absorbed differently by the body. Our survey results indicate that melatonin users are at least three times more likely to use capsules, tablets, or gummies than they are any other type of formulation.
There also isn’t any information on how melatonin affects the body long-term. Experts recommend melatonin use for up to 3 months at a time.
What Happens if You Take Too Much Melatonin?
It’s unlikely that you’ll have a life-threatening reaction to a melatonin overdose. Generally, melatonin isn’t bad for you. Melatonin is a hormone that your body naturally produces, so if you take too much your body just has an excess supply that will take longer than normal for it to process.
Researchers haven’t found a lethal dose of melatonin . However, if you take too much, you may experience unpleasant—though non-serious—side effects.
Symptoms of a Melatonin Overdose
A life-threatening melatonin overdose is rare, especially in adults. But melatonin supplements with higher doses can cause adverse reactions and side effects, including:
- Nightmares
- Headaches
- Irritability
- Stomach pain
- Nausea
- Daytime tiredness
- Dizziness
- Short-term depression symptoms
In our survey, the most commonly reported symptoms included daytime drowsiness (24%), vivid dreams or nightmares (17%), headache (15%), and difficulty waking up (15%). Half said they’d never experienced any of the listed side effects.
It’s important to note, though, that these are known side effects and not necessarily indications of an overdose. Drug overdose symptoms that require immediate emergency medical attention include difficulty breathing, seizures, or a loss of consciousness.
What to Do if You’re Experiencing Melatonin Overdose Symptoms
If you suspect you or someone else is experiencing a melatonin overdose, contact a poison control center. You can talk to a poison expert atPoisonHelp.org or by calling (800) 222-1222 in the U.S.
If you or someone else is experiencing severe symptoms, such as difficulty breathing, seizures, or a loss of consciousness, immediately call 9-1-1 or go to the emergency room. Ingesting melatonin may be particularly dangerous if you’ve consumed other medications or alcohol.
Can Children Overdose on Melatonin?
Experts don’t recommend melatonin for children under 5, and they caution against doses above 3 milligrams for kids 5 and up. Even though melatonin for kids is available without a prescription in the U.S., you shouldn’t give melatonin to a child without discussing it with their doctor first.
Children can experience side effects of melatonin overdose, but serious symptoms are rare and experts haven’t found a lethal melatonin dose for adults or children. Kids produce more melatonin than adults do naturally, so it’s important to keep dosage low. If children ingest more melatonin than their body can process, they may experience the following side effects.
- Nightmares
- Headaches
- Irritability
- Stomach pain
- Nausea
- Daytime tiredness
- Dizziness
- Bedwetting
Melatonin supplements are sometimes used to treat children who have insomnia, other sleep disorders, or neurodevelopmental disorders, like autism, attention-deficit hyperactivity disorder (ADHD), or epilepsy. Lower doses are thought to be safer and more effective than higher doses.
What Is the Treatment for a Melatonin Overdose?
There’s no specific antidote for a melatonin overdose, and treatment typically focuses on managing symptoms. In most cases, mild melatonin overdoses can be treated at home by stopping use and allowing the supplement to naturally clear from the body.
Don’t attempt to induce vomiting if you suspect a melatonin overdose. Instead, wait in a safe place for symptoms to pass. Common symptoms, such as drowsiness, headache, nausea, or dizziness, often resolve within a few hours.
If symptoms are more severe or prolonged, medical attention may be necessary. A healthcare provider may recommend supportive care, such as hydration, rest, or monitoring heart rate and blood pressure if irregularities are present.
In rare cases, especially when melatonin is taken in very high doses or combined with other medications, evaluation at a hospital or poison control center may be needed to ensure safety. If you experience difficulty breathing, loss of consciousness, or seizures, call 9-1-1 or go to the emergency room. You can also talk to an expert at PoisonHelp.org.
When Should I Talk With a Doctor?
Although melatonin has largely been found to be safe, talk to your doctor before beginning to take it or any dietary supplement. People often assume dietary supplements are safe, but they aren’t tested by the FDA for quality or accuracy, like prescription drugs are. Survey responses show that nearly 34% of people don’t seek out third-party researchers before buying a sleep aid.
Supplements may also cause side effects or interact with prescription drugs. Melatonin effects on pregnant and post-partum people haven’t been significantly studied. Speak with a doctor if you’re pregnant or nursing.
If you’re taking melatonin and experience serious side effects or are concerned about overdose, call poison control or seek emergency medical attention immediately.
Frequently Asked Questions
How long do melatonin side effects last?
Melatonin side effects—such as grogginess, dizziness, headache, or nausea—usually resolve within a few hours as the supplement leaves your system. The exact duration can depend on the dose taken, your metabolism, and whether melatonin was combined with other substances like alcohol or sedating medications. In most cases, side effects are mild and temporary.
If symptoms persist longer than a few hours or are severe, it’s best to contact a healthcare professional.
What are the long-term effects of taking melatonin?
In the short-term, you can take melatonin every night, but long-term use hasn’t been widely studied. Most studies have only followed people using melatonin for about a month. Although longer-term studies haven’t found serious adverse events from using melatonin, experts say there isn’t enough research available to conclude that long-term use of melatonin is safe.
Can you build a tolerance to melatonin?
Melatonin does not typically lead to physical dependence or tolerance in the way that some sleep medications do. However, some people may feel that melatonin becomes less effective over time, especially if taken in high doses or used nightly without addressing the root cause of sleep issues. This reduced effectiveness may be due to changes in your body’s natural melatonin production or sleep patterns rather than true tolerance.
If melatonin seems to stop working, it’s a good idea to take a break or consult a healthcare provider to explore other sleep strategies.
What shouldn’t you take with melatonin?
You should avoid taking melatonin with alcohol, caffeine, and certain prescription medications. Alcohol and caffeine can affect your sleep-wake cycle and impact natural melatonin production. Birth control may increase natural melatonin production, too, so taking a melatonin supplement alongside birth control could result in more melatonin than your body can process
.
Certain anxiety and depression medications can have interactions with melatonin, including some SSRIs and sedatives. Melatonin can boost your immune system, so if you’re taking immunosuppressants, you may want to avoid melatonin. Melatonin can also interfere with prescription drugs that are used to treat sleep disorders.
Consult your physician before taking melatonin, especially if you take other prescription medications.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
11 Sources
-
Besag, F., Vasey, M. J., Lao, K., & Wong, I. (2019). Adverse events associated with melatonin for the treatment of primary or secondary sleep disorders: A systematic review. CNS Drugs, 33(12), 1167–1186.
https://pubmed.ncbi.nlm.nih.gov/31722088/ -
Freeman, D., Lind, J., Weidle, D., et al. Centers for Disease Control and Prevention. (2024, March 7). Emergency Department Visits for Unsupervised Pediatric Melatonin Ingestion – United States, 2019-2022. Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention.
https://www.cdc.gov/mmwr/volumes/73/wr/pdfs/mm7309a5-H.pdf -
Neubauer, D. (2024, March). Pharmacotherapy for insomnia in adults. In R. Benca, J. Elmore, & A. Eichler (Ed.). UpToDate.
https://www.uptodate.com/contents/pharmacotherapy-for-insomnia-in-adults -
Shenoy P, Etcheverry A, Ia J, Witmans M, Tablizo MA. Melatonin Use in Pediatrics: A Clinical Review on Indications, Multisystem Effects, and Toxicity. Children. 2024; 11(3):323.
https://www.mdpi.com/2227-9067/11/3/323 -
Cohen, P. A., Avula, B., Wang, Y. H., Katragunta, K., & Khan, I. (2023). Quantity of Melatonin and CBD in Melatonin Gummies Sold in the US. JAMA, 329(16), 1401–1402.
https://pubmed.ncbi.nlm.nih.gov/37097362/ -
Savage, R., Zafar, N., Yohannan, S., & Miller, J. (2022, August 8). Melatonin. StatPearls.
https://www.ncbi.nlm.nih.gov/books/NBK534823/ -
Savage, R., Zafar, N., Yohannan, S., & Miller, J. (2024, February 9). Melatonin. StatPearls.
https://www.ncbi.nlm.nih.gov/books/NBK534823/ -
Tuft, C., Matar, E., Menczel Schrire, Z., Grunstein, R. R., Yee, B. J., & Hoyos, C. M. (2023). Current Insights into the Risks of Using Melatonin as a Treatment for Sleep Disorders in Older Adults. Clinical interventions in aging, 18, 49–59.
https://pubmed.ncbi.nlm.nih.gov/36660543/ -
Shenoy, P., Etcheverry, A., Ia, J., WItmans, M., & Tablizo, M. (2024, March 9). Melatonin Use in Pediatrics: A Clinical Review of Indications, Multisystem Effects, and Toxicity. Children, 11, 323.
https://www.mdpi.com/2227-9067/11/3/323 -
Besag, F. M. C., Vasey, M. J., Lao, K. S. J., & Wong, I. C. K. (2019). Adverse Events Associated with Melatonin for the Treatment of Primary or Secondary Sleep Disorders: A Systematic Review. CNS drugs, 33(12), 1167–1186.
https://pubmed.ncbi.nlm.nih.gov/31722088/ -
Webley, G. E., & Leidenberger, F. (1986). The circadian pattern of melatonin and its positive relationship with progesterone in women. The Journal of Clinical Endocrinology and Metabolism, 63(2), 323–328.
https://pubmed.ncbi.nlm.nih.gov/3722324/




















