REM Sleep: What It Is and Why It’s Important
- What Is REM Sleep?
- What Happens During REM Sleep?
- When Does REM Sleep Occur?
- Why Is REM Sleep Important?
- How Much REM Sleep Do You Need?
- What Happens if You Don’t Get Enough REM Sleep?
- How Can You Improve Your REM Sleep?
- What Sleep Disorders Are Associated With REM Sleep?
- When Should You Talk to Your Doctor?
- Rapid eye movement or REM sleep is the fourth and final stage of sleep and is when you have your most vivid and intense dreams.
- REM sleep is characterized by increased brain activity, limited muscle movement, darting eye movement, and fluctuating respiration and heart rate.
- Most adults need about two hours of REM sleep each night, which contributes to brain function, memory consolidation, and emotional health.
Rapid eye movement (REM) sleep is best known for its association with vivid dreaming, and it’s true that you tend to have the most intense dreams during this sleep stage. But REM sleep has importance far beyond dreaming—from brain development to emotional regulation.
Although some aspects of REM sleep are still being investigated, studies have gradually expanded what we know about this unique sleep stage. Below, we’ll explore what we know about REM sleep, including how much REM sleep we need, why we need it, and how to get more.
Looking to improve your sleep? Try upgrading your mattress.
What Is REM Sleep?
Rapid eye movement (REM) sleep is one of four stages of sleep. During REM sleep, many aspects of brain and body activity ramp up, at times almost to the same level as when you’re awake .
REM sleep was first discovered in the 1950s, when scientists studying sleeping infants noticed distinct periods when their eyes darted quickly from side to side behind closed eyelids. These rapid eye movements earned REM sleep its name.
Over time, researchers have gathered more and more data about REM sleep, including the fact that it’s the sleep stage with the most active dreaming . REM sleep has also been detected in many mammals and other animals, highlighting its evolutionary importance.
In people, sleep labs with specialized equipment allow researchers to see what happens when you’re asleep that makes REM sleep different from the other stages.
Tracking REM Sleep
According to a SleepFoundation.org survey, about half of the people who use a sleep tracker consistently review the amount of REM sleep they get each night.
While consumer sleep trackers can’t perfectly measure sleep stages, they can still help identify trends over time and encourage healthier sleep habits. If your device shows consistently low REM sleep, it may be worth evaluating your sleep routine or talking to your doctor.
What Happens During REM Sleep?
During REM sleep, your eyes move rapidly behind your closed eyelids. This is one of the only visible external signs of REM sleep, but inside the brain and body, a lot more is happening :
- Your brain activity ramps up, often leading to vivid dreams
- Most of your muscles become temporarily paralyzed
- Your pulse and breathing speed up and may become less consistent
Compared to other stages of sleep, REM sleep involves heightened activity that in many ways resembles wakefulness. That said, you remain asleep, and most of your body loses muscle tone. Although we still don’t know for sure why this happens, many researchers believe this temporary paralysis helps protect us from acting out our dreams.
When Does REM Sleep Occur?
You experience your first period of REM sleep about 60 to 90 minutes after falling asleep.
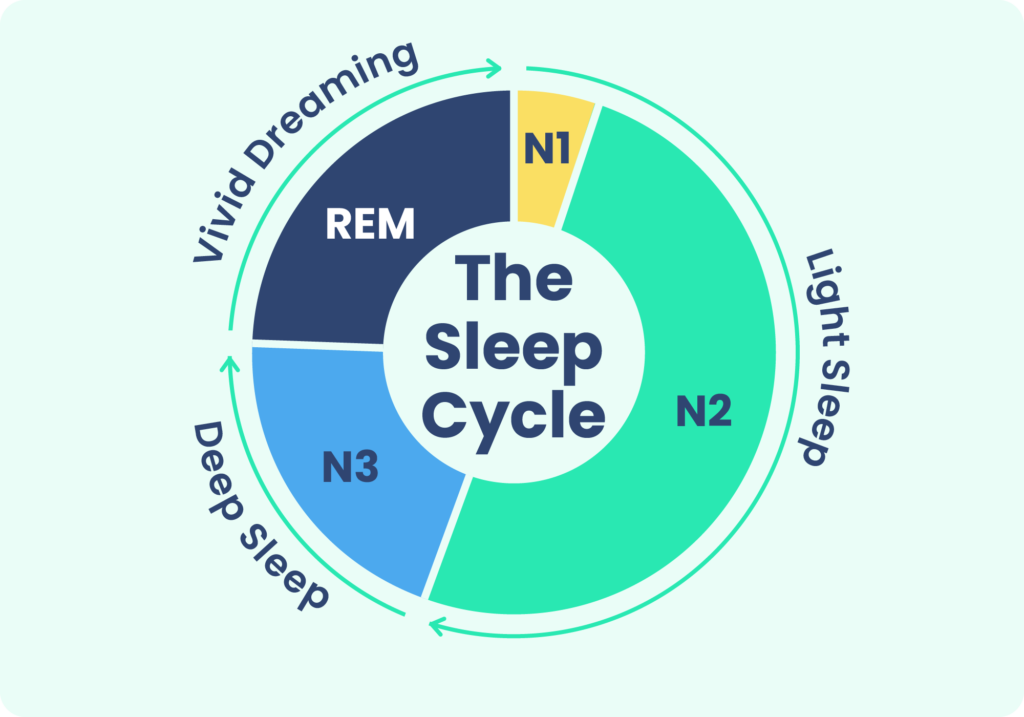
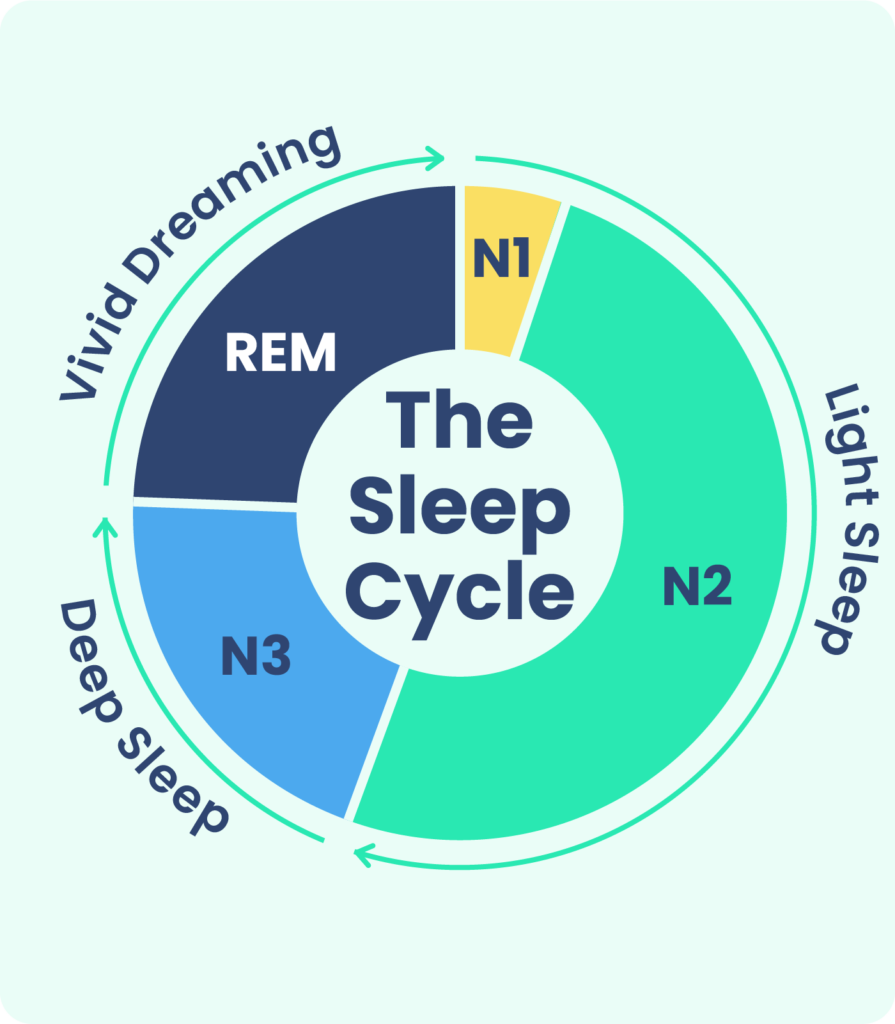
During a full night’s sleep, you cycle through different stages of sleep multiple times. There are four stages, including REM sleep and three stages of non-REM sleep. A full sleep cycle takes about 90 to 120 minutes to complete.
With each new cycle, you spend increasing amounts of time in REM sleep, so most of your REM sleep takes place in the second half of the night. Activity levels in your brain and body change during each stage of sleep:
- Stage 1 (Light Sleep): In stage 1, you’re just dozing off. Your brain and body start to relax, but you can still be easily awoken.
- Stage 2 (Light Sleep): In stage 2, your body and brain slow down even more. Your heart rate, body temperature, and breathing all decrease, and your muscles relax.
- Stage 3 (Deep Sleep): During deep sleep, your brain and body slow down the most. In this restorative sleep stage, your body physically repairs itself, boosting your immune system and supporting your bones, muscles, and tissue. It can be difficult to wake you up during stage 3 sleep.
- Stage 4 (REM Sleep): Your brain activity in this stage is similar to how it is when you’re awake. You experience a loss of most muscle activity, but your eyes move quickly underneath your eyelids.
Although the sleep stages are described numerically, you don’t always progress through them in this exact order. For example, in many sleep cycles, you transition from stage 3 sleep back to stage 2 sleep before beginning a period of REM sleep.
REM vs. Non-REM Sleep
REM sleep is one of the most fascinating stages of sleep because it’s so different from the other stages. Traits unique to REM sleep that differentiate it from non-REM sleep include:
- Brain wave activity that’s more similar to wakefulness than non-REM sleep
- Temporary paralysis of most muscles compared to relaxed but movable muscles in non-REM sleep
- Irregular breathing and heart rate instead of the steady, slower breathing and pulse during non-REM sleep
- Steady movement of the eyes compared to minimal eye movement in non-REM sleep
Why Is REM Sleep Important?
REM sleep is a core part of how sleep works, so spending enough time in the REM stage is an important part of getting a healthy night’s sleep. It also plays a role in many specific aspects of physical and mental health in both the short and long term.
- Brain Function and Development: While you’re in REM sleep, your brain is on cleanup duty to remove cellular waste . That helps set you up for better brain function and thinking the next day. REM sleep also promotes brain development, which is why researchers think newborns spend most of their sleep time in REM .
- Dreaming: A majority of your dreams take place during REM sleep, and dreams during REM tend to be more vivid. However, REM is not the only stage in which dreams occur — that’s actually a common sleep myth.
- Emotional Processing: Dreaming and the brain activity during REM sleep play a role in how we process emotions. Consistent REM sleep helps with emotional regulation and our response to difficult events , and disrupted REM sleep has been associated with a worse mood and mental health conditions like depression and post-traumatic stress disorder (PTSD) .
- Memory Consolidation: REM sleep strengthens connections between brain regions, and some studies suggest it sharpens your working memory . During the REM stage, your brain reviews things you’ve learned recently, deciding which items to keep in your memory and which to delete. That said, some memory consolidation also takes place in deep sleep , which reinforces the benefits of a complete night’s sleep.
- Wakefulness Preparation: By ramping up activity in the body, REM sleep may help us get ready to wake up refreshed. This heightened activity during REM sleep is also believed to help protect the cardiovascular system from a sudden surge in activity upon waking up .
How Much REM Sleep Do You Need?
In adulthood, most people need about two hours of REM sleep each night. But infants and children need more REM sleep, because their brains are still rapidly developing. For example, newborn babies spend around eight hours in REM sleep each day.
How much time you actually spend in REM sleep can vary from night to night. On a night when you’re short of sleep, your total REM time can get cut short. This can trigger your brain to initiate more REM sleep the following night, which is known as a REM rebound . Some research also suggests that REM sleep may increase after learning new information.
What Happens if You Don’t Get Enough REM Sleep?
Because REM sleep enables better brain function, memory, and emotional regulation, a lack of REM sleep can cause a range of issues. On top of that, a lack of REM sleep circumvents healthy sleep overall, contributing to sleep deprivation. In the short term, signs of sleep deprivation can include :
- Difficulty concentrating
- Excessive daytime sleepiness
- Forgetfulness or poor memory
- Irritability or frustration
- Greater risk of accidents
Over the long term, insufficient sleep can weaken your immune system and raise your risk of conditions like heart disease, diabetes, depression, and anxiety.
How Can You Improve Your REM Sleep?
If you want to get more REM sleep, your first step should be to shore up the quantity and quality of your overall sleep. If you’re not getting enough sleep each night, the odds are that you’re spending less time in REM than you need.
To avoid this, start by adopting healthy sleep habits that reinforce your sleep hygiene. One important way to do this is to maintain a consistent sleep schedule that budgets enough time for a full seven to nine hours of total sleep. This helps reinforce your body’s internal clock, or circadian rhythm, which is essential in regulating your REM sleep.
You also want to avoid too much artificial light at night, whether from overhead lights, lamps, or screens. This isn’t just because it’s easier to fall asleep in a dark room. Too much light at night can disrupt your circadian rhythm and interfere with quality REM sleep .
Other ways to get better REM sleep are based on eliminating factors that short-circuit normal sleep cycles. Things that can throw off REM sleep include:
- Excess stress
- Consumption of alcohol or cannabis at night
- Taking certain medications, including some sleep aids
Many sleep disorders, including insomnia and sleep apnea, can prevent you from getting adequate REM sleep. For that reason, it’s important to talk with a doctor if you have ongoing or worsening sleep problems or symptoms of an underlying sleep disorder.
Using Sleep Data to Get More REM Sleep
Many people use sleep-tracker data to make meaningful changes to their nightly routines—and REM sleep is often a key focus. These behavioral changes can lead to deeper, more restorative sleep and longer periods of REM. The graph below highlights some of the most common adjustments people report making based on sleep-tracker insights.
What Sleep Disorders Are Associated With REM Sleep?
Not everyone has typical patterns of REM sleep. Certain sleep disorders are associated with abnormal REM sleep.
- REM Sleep Behavior Disorder (RBD): Some nights, people with REM Sleep Behavior Disorder don’t experience the expected temporary muscle paralysis when they enter REM sleep. As a result, they may act out their dreams, such as by shouting, punching, kicking, or jerking in their sleep. This can lead to injuries to themselves or their partners. RBD has been found to frequently precede neurodegenerative disease.
- Narcolepsy:Narcolepsy is a rare condition of extreme daytime sleepiness, and it may also involve temporary losses of muscle control while awake. People with narcolepsy have abnormal REM sleep patterns, including a tendency to quickly enter REM after falling asleep .
- Nightmare Disorder: A person with nightmare disorder regularly experiences intense and distressing nightmares. These bothersome nightmares arise during periods of REM sleep.
- Obstructive Sleep Apnea (OSA) and Central Sleep Apnea (CSA): Although breathing disruptions from sleep apnea do not occur exclusively during REM sleep, they do affect how much REM sleep you get. People with sleep apnea have fragmented sleep cycles, which can reduce their ability to get adequate and consistent REM sleep.
- Insomnia: Like sleep apnea, insomnia can cause fragmented and restless sleep. As a result, people with insomnia may struggle to get enough high-quality REM sleep.
- Insufficient Sleep Syndrome (ISS): ISS is when a person voluntarily cuts their sleep short, such as for work or social activities. Because they don’t get enough total sleep, people with ISS often have reduced REM sleep time.
When Should You Talk to Your Doctor?
You should talk to your doctor if you’re having any sleep problems that are severe, long-lasting, or getting worse. If you notice that poor sleep is affecting you when you’re awake, your doctor may be able to help.
Working with a doctor can help determine if you have any underlying sleep disorder or if there is another cause of your difficulty sleeping. Based on that, they can help develop a treatment approach to improve your sleep.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
19 Sources
-
Peever, J., & Fuller, P. M. (2017). The biology of REM sleep. Current Biology, 27(22), R1237-R1248.
https://pubmed.ncbi.nlm.nih.gov/29161567/ -
Blumberg, M. S., Lesku, J. A., Libourel, P. A., Schmidt, M. H., & Rattenborg, N. C. (2020). What is REM sleep?. Current Biology, 30(1), R38–R49.
https://pubmed.ncbi.nlm.nih.gov/31910377/ -
Schwab, R. J. (2022, September). Overview of sleep. Merck Manual Consumer Version.
https://www.merckmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/overview-of-sleep -
What happens during sleep? Eunice Kennedy Shriver National Institute of Child Health and Human Development.
https://www.nichd.nih.gov/health/topics/sleep/conditioninfo/what-happens. -
Feriante, J., & Araujo, J. F. (2021). Physiology, REM sleep. In StatPearls. StatPearls Publishing.
https://pubmed.ncbi.nlm.nih.gov/30285349/ -
Patel, A. K., Reddy, V., Shumway, K. R., Araujo, J. F. (2024, January 26). Physiology, sleep stages. StatPearls.
https://www.ncbi.nlm.nih.gov/books/NBK526132/ -
Di T, Zhang L, Meng S, et al. The impact of REM sleep loss on human brain connectivity. Transl Psychiatry. 2024;14(1):270. Published 2024 Jul 2. doi:10.1038/s41398-024-02985-x
https://pubmed.ncbi.nlm.nih.gov/38956035/ -
Miller KE, Gehrman PR. REM Sleep: What Is It Good For?. Curr Biol. 2019;29(16):R806-R807. doi:10.1016/j.cub.2019.06.074
https://pubmed.ncbi.nlm.nih.gov/31430480/ -
Naiman R. Dreamless: the silent epidemic of REM sleep loss. Ann N Y Acad Sci. 2017;1406(1):77-85. doi:10.1111/nyas.13447
https://pubmed.ncbi.nlm.nih.gov/28810072/ -
Lau, E. Y., Wong, M. L., Lau, K. N., Hui, F. W., & Tseng, C. H. (2015). Rapid-eye-movement-sleep (REM) associated enhancement of working memory performance after a daytime nap. PloS One, 10(5), e0125752.
https://pubmed.ncbi.nlm.nih.gov/25970511/ -
Ackermann, S., & Rasch, B. (2014). Differential effects of non-REM and REM sleep on memory consolidation?. Current Neurology and Neuroscience Reports, 14(2), 430.
https://pubmed.ncbi.nlm.nih.gov/24395522/ -
National Heart, Lung, and Blood Institute. How Sleep Works – Why Is Sleep important? National Heart, Lung, and Blood Institute. Published March 24, 2022.
https://www.nhlbi.nih.gov/health/sleep/why-sleep-important -
Feriante, J. & Singh, S. (2023 October). REM Rebound Effect. StatPearls.
https://www.ncbi.nlm.nih.gov/books/NBK560713/ -
Rasch, B., & Born, J. (2013). About sleep’s role in memory. Physiological Reviews, 93(2), 681–766.
https://pubmed.ncbi.nlm.nih.gov/23589831/ -
A.D.A.M. Medical Encyclopedia. (2020, August 13). Sleep and your health. MedlinePlus.
https://medlineplus.gov/ency/patientinstructions/000871.htm -
Grandner, M. A., Patel, N. P., Gehrman, P. R., Perlis, M. L., & Pack, A. I. (2010). Problems associated with short sleep: Bridging the gap between laboratory and epidemiological studies. Sleep Medicine Reviews, 14(4), 239–247.
https://pubmed.ncbi.nlm.nih.gov/19896872/ -
Barbato G. REM Sleep: An Unknown Indicator of Sleep Quality. Int J Environ Res Public Health. 2021;18(24):12976. Published 2021 Dec 9. doi:10.3390/ijerph182412976
https://pubmed.ncbi.nlm.nih.gov/34948586/ -
Schwab, J. (2022 September). Narcolepsy. Merck Manual Consumer Version.
https://www.merckmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/narcolepsy -
Gieselmann A, Ait Aoudia M, Carr M, et al. Aetiology and treatment of nightmare disorder: State of the art and future perspectives. J Sleep Res. 2019;28(4):e12820. doi:10.1111/jsr.12820
https://pubmed.ncbi.nlm.nih.gov/30697860/











