When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Sleep Paralysis Demon
At a Glance
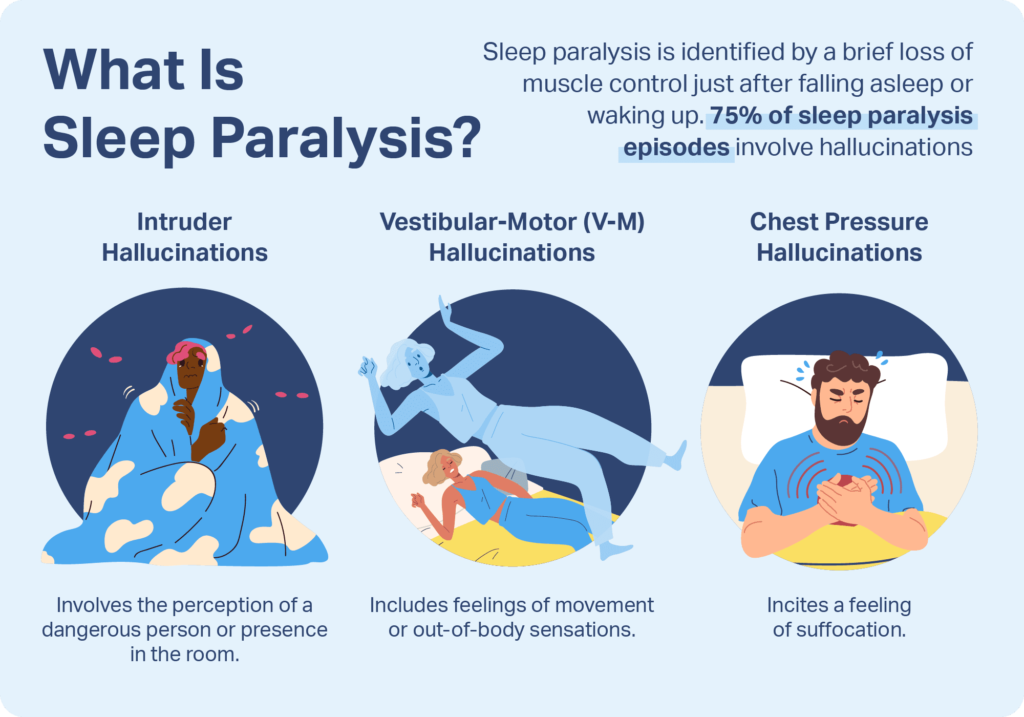
Sleep paralysis demons refer to the vivid, often terrifying hallucinations that some people experience during episodes of sleep paralysis—a state where the body is temporarily unable to move while falling asleep or waking up. During this state, individuals may feel a heavy pressure on their chest, sense a threatening presence in the room, or even see shadowy figures, commonly described as “demons” or intruders.
Sleep demons are frightening phenomena that are all too real for people who experience sleep paralysis. Roughly 20% of people have an episode of sleep paralysis at least occasionally. In as many as 75% of these episodes, the sleeper has a hallucination in which they hear, see, feel, or sense something in their bedroom that is not actually there.
Below, we’ll explore the fascinating topic of sleep demons, including various cultural depictions of these intruders, modern scientific explanations, and ways to reduce the risk of sleep paralysis.
What Is Sleep Paralysis?
As a person drifts off to sleep, their body begins to cycle through two types of sleep: rapid eye movement (REM) sleep and non-rapid eye movement (NREM) sleep. During REM sleep there is a heightened level of activity in the brain, and breathing, blood pressure, and heart rate increase. This is also the type of sleep characterized by rich and detailed dreams and nightmares.
Paradoxically, during REM sleep, the body enters a state of temporary paralysis called muscle atonia. This state is likely a mechanism to prevent sleepers from injuring themselves by acting out their dreams.
In sleep paralysis, the lines between sleep and wakefulness become blurred. As a person is at the edge of waking up or falling asleep, they become aware of their surroundings while their muscle paralysis continues for a few seconds to several minutes. This means that they can think, see, and breathe while they lie awake, but they are unable to move their body.
Sleep paralysis is most often triggered by a lack of sleep. When sleep paralysis occurs in people who have no other underlying medical condition, it’s called isolated sleep paralysis.
What Is a Sleep Paralysis Demon?
When sleep paralysis is accompanied by a sleep-related hallucination, the person then begins to see, hear, feel, or sense changes in their environment that do not actually exist . These are referred to as sleep paralysis demons.
During this state, it’s common to feel a heavy weight on the chest, a sense of being watched, or to see shadowy, human-like figures in the room. These figures are often interpreted as demons, ghosts, or intruders due to their menacing presence and the intense fear they provoke. While the experience can feel supernatural, most researchers have come to the conclusion that these “demons” are actually the brain’s way of trying to make sense of being conscious while still partially in a dream state.
Looking to improve your sleep? Try upgrading your mattress.
Types of Sleep Paralysis Demons
Hallucinations may be simple, stationary images or more complex and multi-sensory intruder, incubus, or vestibular-motor hallucinations.
- The Intruder: A shadowy figure or presence that feels menacing. People often describe seeing someone standing in the corner, lurking near the bed, or approaching slowly.
- The Incubus: A sensation of pressure on the chest, as if someone is sitting or lying on top of the sleeper. This often comes with difficulty breathing and feelings of dread.
- The Shadow Person: Dark, faceless silhouettes that seem to watch or move around the room. They don’t always interact with the person but evoke a deep fear due to their appearance and presence.
- The Witch or Old Hag: A specific figure, often described as a crone or witch-like being, sitting on the chest or standing nearby. This type is especially common in folklore and historical accounts of sleep paralysis.
- Out-of-Body Figures or Doppelgängers: Less common but reported, these involve seeing a version of oneself or floating figures near the body, sometimes tied to a feeling of detachment or disorientation.
Dreams vs. Hallucinations
Hallucinations can be hard to distinguish from dreams, but several differences make these two phenomena distinct.
- Awareness: People experiencing sleep paralysis are typically aware that they have woken up, while dreamers are most often unaware that they are asleep.
- Setting: While dreams may take place anywhere and often include settings outside of the home, sleep-related hallucinations overlap with reality and take place within a person’s bedroom or real-life sleep environment.
- Emotions: Although some episodes of sleep paralysis may be pleasant or enjoyable, up to 90% of hallucinations during sleep paralysis involve feelings of fear. By contrast, only around 30% of dreams can be considered frightening.
- Recall: Many people forget their dreams after waking, but people with nighttime hallucinations often recall the experience vividly.
Cultural Depictions of Sleep Demons
While modern scientists consider sleep demons to be hallucinations, this is not the first or only interpretation of this phenomenon. Societies throughout history have developed their own explanations for these experiences, each stemming from a unique cultural context.
- Lilitu: Some of the earliest writing related to sleep paralysis comes from Mesopotamia around 2400 BC. These accounts refer to Lilitu, a female demon. Researchers believe that it is from this early folklore that the concepts of incubus, succubus, and the night-mare descended.
- Night-mare: In Europe during the middle ages, the term night-mare referred to a supernatural entity, typically female, that positioned herself on top of a person’s chest to suffocate them. Medical explanations up to the 20th century suggested that a night-mare was caused by stagnant blood or vapors rising from the stomach and affecting the nervous system.
- Ag rog: The old hag phenomenon , also called ag rog, was described by residents of Newfoundland in the 1970s. Believers attribute paralysis, pressure on the chest, and other symptoms to blood that has stagnated, excessive work, or an enemy who wants to harm the sleeper.
- Pisadeira: In Brazilian folklore, a pisadeira is an old woman who lies in wait on roofs and walks on the chests of people who sleep on their back with a full stomach.
- Kanashibari:Kanashibari is a Japanese name for an experience between sleep and wakefulness involving paralysis, fear, anxiety, and sometimes hallucinations. The term kanashibari comes from a similar-sounding word that describes the magical powers of a Buddhist deity, which monks were believed to be capable of harnessing to paralyze others.
- Jinn: Some in Egypt attribute sleep paralysis to Jinn , which are supernatural creatures associated with witchcraft, madness, and nightmares. These creatures are said to be able to terrify or possess a sleeping person.
- Khmaoch sângkât: In Cambodian refugees, sleep paralysis may be described using the Khmer phrase khmaoch sângkât, which describes a supernatural being pushing down on the sleeper’s chest or neck. Hallucinations may include a ghost dispatched by a sorcerer, a demon wanting to cause fear, or a person who died during the Cambodian genocide.
What Causes a Sleep Paralysis Demon?
Although the exact cause of sleep-related hallucinations remains unknown, many experts believe that hallucinations during sleep paralysis occur when people experience the vivid dreams of REM sleep while they are awake.
To explain the often frightening experiences during these hallucinations, researchers have considered the role of hormones, mirror neurons, changes in breathing, and the survival centers of the brain.
- Presence of serotonin: As a person begins to wake up, hormones like serotonin suppress REM sleep and contribute to increased awareness of the person’s surroundings. But during an episode of sleep paralysis, serotonin is released while a person remains stuck in REM sleep. This may induce hallucinations and activate fear circuits in the brain.
- Brain disturbances: Malfunctions in parts of the brain responsible for creating an image of the body may underlie the creation of human-like figures often seen during a hallucination. These disturbances may also be responsible for the sexual nature of some hallucinations, as well as for the phantom movements and pain that sleepers may feel in their limbs.
- Breathing changes: When major muscles become paralyzed during REM sleep, a person’s breathing normally grows more shallow. Becoming aware of diminished breathing during an episode of sleep paralysis may explain the feelings of suffocation or pressure on the chest that people describe during a sleep-related hallucination.
- Cycles of fear and panic: As a person begins to realize that they cannot move despite their alarming perceptions, their fear may escalate and trigger panic or a fight-or-flight response. This in turn may exacerbate the frightening content of their hallucinations.
How Can You End an Episode of Sleep Paralysis?
Finding ways to interrupt episodes as they are happening is an important coping strategy for people with sleep paralysis. Potential ways for escaping an episode of sleep paralysis include:
- Attempting to move the arms, legs, or torso
- Trying to move the mouth or eyes
- Being touched by another person
- Being roused by an alarm clock
- Focusing on relaxing the body and mind
- Mentally reciting a mantra or prayer
Researchers have proposed that lucid dreaming may be another way for people to gain control over their sleep paralysis. Although more research is needed, learning methods for lucid dreaming may help people turn frightening hallucinations into more neutral or positive experiences.
What Can You Do to Prevent Sleep Paralysis Demons?
To prevent sleep paralysis and associated hallucinations, consider ways to address any underlying triggers for episodes.
- Learn about sleep paralysis: Understanding what is happening in the body during sleep-related hallucinations can reduce the confusion and fear they cause. Many people feel less afraid once they understand that hallucinations are alarming but harmless.
- Do not ignore fear and anxiety: Anxiety may increase the risk of poor sleep and sleep paralysis. Conversely, sleep paralysis can itself cause anxiety. To interrupt this cycle, consider talking to your doctor or a mental health professional about ways to manage fear and anxiety.
- Relax before bed: Not only does relaxation help you sleep better, it may also reduce the chances of having an episode of sleep paralysis.
- Change sleeping position: Research suggests that shifting how you sleep may also help prevent episodes of sleep paralysis. For instance, if you are a back sleeper, try sleeping on your side or stomach instead.
- Improve your sleep hygiene: Since sleep paralysis is linked to other sleep issues, improving your sleep hygiene may help reduce episodes. Maintain a consistent sleep schedule, create a relaxing nightly routine, and avoid things that interfere with sleep, like caffeine, alcohol, and the bright lights created by electronics.
- Start a sleep journal: Consider starting a sleep diary to record both nighttime sleep issues and daytime symptoms. Tracking these experiences over time may help you pinpoint the early signs of sleep paralysis and lead to a more helpful conversation with your doctor.
- Try cognitive-behavioral therapy: Cognitive-behavioral therapy for sleep paralysis focuses on improving your sleep habits, teaching relaxation techniques to manage recurring episodes, and helping you stay calm during scary hallucinations. It may also include practicing how to interrupt episodes when they happen, working through anxious thoughts, and mentally rehearsing positive ways to handle sleep paralysis when it occurs .
Perhaps the most important way to prevent sleep-related hallucinations is to talk to your doctor. Having an honest and open dialogue allows a doctor to accurately assess your condition, provide education, and recommend the best treatment approach.
Frequently Asked Questions
Are sleep paralysis demons real?
No, sleep paralysis demons are not real. They’re hallucinations your brain creates while your body is stuck between sleep and wakefulness.
Is sleep paralysis dangerous?
Sleep paralysis isn’t dangerous, but it can be very unsettling. It usually passes on its own and doesn’t cause physical harm.
How long does sleep paralysis last?
Most episodes last anywhere from a few seconds to a couple of minutes before movement returns. It may feel longer in the moment.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
11 Sources
-
Scammell, T. E. (2022, June 12). Clinical features and diagnosis of narcolepsy in adults. In R. Benca (Ed.). UpToDate.
https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-narcolepsy-in-adults -
American Academy of Sleep Medicine. (2014). The International Classification of Sleep Disorders – Third Edition (ICSD-3). Darien, IL.
https://aasm.org/ -
Khan AA, Abid A, Nawaz M, et al. Experiences and beliefs related to sleep paralysis among the general population of the twin cities: A cross-sectional study. Sleep Med. 2024;124:146-153. doi:10.1016/j.sleep.2024.09.022
https://www.sciencedirect.com/science/article/abs/pii/S1389945724004453 -
Cox, A. M. (2015). Sleep paralysis and folklore. JRSM Open, 6(7), 2054270415598091.
https://pubmed.ncbi.nlm.nih.gov/28008370/ -
Davies, O. (2003). The nightmare experience, sleep paralysis, and witchcraft accusations. Folklore, 114(2), 181–203.
https://www.tandfonline.com/doi/abs/10.1080/0015587032000104211 -
Ness, R. C. (1978). The Old Hag phenomenon as sleep paralysis: A biocultural interpretation. Culture, Medicine and Psychiatry, 2(1), 15–39.
https://pubmed.ncbi.nlm.nih.gov/699620/ -
de Sá, J. F., & Mota-Rolim, S. A. (2016). Sleep paralysis in Brazilian folklore and other cultures: A brief review. Frontiers in Psychology, 7, 1294.
https://pubmed.ncbi.nlm.nih.gov/27656151/ -
Fukuda, K., Miyasita, A., Inugami, M., & Ishihara, K. (1987). High prevalence of isolated sleep paralysis: Kanashibari phenomenon in Japan. Sleep, 10(3), 279–286.
https://pubmed.ncbi.nlm.nih.gov/3629091/ -
Jalal, B., & Hinton, D. E. (2013). Rates and characteristics of sleep paralysis in the general population of Denmark and Egypt. Culture, Medicine and Psychiatry, 37(3), 534–548.
https://pubmed.ncbi.nlm.nih.gov/23884906/ -
Hinton, D. E., Pich, V., Chhean, D., & Pollack, M. H. (2005). ‘The ghost pushes you down’: Sleep paralysis-type panic attacks in a Khmer refugee population. Transcultural Psychiatry, 42(1), 46–77.
https://pubmed.ncbi.nlm.nih.gov/15881268/ -
Bhalerao V, Gotarkar S, Vishwakarma D, Kanchan S. Recent Insights Into Sleep Paralysis: Mechanisms and Management. Cureus. 2024;16(7):e65413. Published 2024 Jul 26. doi:10.7759/cureus.65413
https://pmc.ncbi.nlm.nih.gov/articles/PMC11344621/











