When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Depression and Sleep
If you or someone you know is in crisis, dial 988 to reach the Suicide and Crisis Lifeline, which provides 24/7, free, and confidential support.
- Sleep and depression are closely linked, and lack of sleep can worsen depression.
- Symptoms of depression can include troubling thoughts, irritable mood, difficulty concentrating, and a lack of energy.
- Treating sleep problems can help alleviate depressive symptoms.
Depression is marked by persistent bouts of sadness, disappointment, and hopelessness, as well as other emotional, mental, and physical changes that lead to difficulties with daily activities. When difficult emotions remain present for more than two weeks, are felt nearly every day, and remain present for most of the day, they may be related to a group of mood disorders called depressive disorders.
Depression disorders are often accompanied by sleep troubles. People with depression may find it difficult to fall asleep and stay asleep during the night or experience periods of excessive daytime sleepiness.
Understanding the complex relationship between sleep and depression can be an important step in improving sleep quality and better managing depression.
Looking to improve your sleep? Try upgrading your mattress.
How Are Depression and Sleep Related?
Depression and sleep are closely connected. A majority of people with depression experience sleep issues. In fact, doctors may hesitate to diagnose depression in the absence of complaints about sleep .
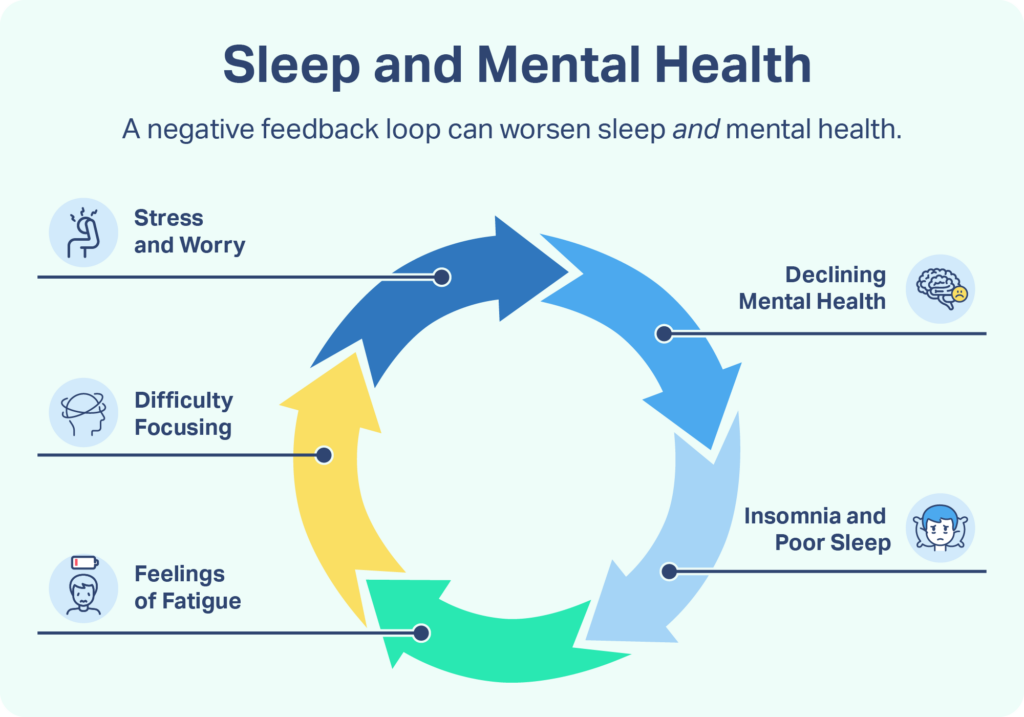
Depression and sleep issues have a bidirectional relationship . This means that poor sleep can contribute to the development of depression and having depression makes a person more likely to experience sleep troubles. This complex relationship can make it challenging to know which came first, sleep issues or depression.
Sleep Problems Associated With Depression
Sleep issues commonly associated with depression include insomnia, hypersomnia, and obstructive sleep apnea. It is believed that about 20% of people with depression have obstructive sleep apnea and about 15% have hypersomnia.
Sleep issues may influence the function of the neurotransmitter serotonin, which can contribute to the development of depression. Sleep disruptions can affect the body’s stress system, disrupting circadian rhythms and increasing vulnerability for depression .
Depression and Insomnia
Approximately 40% of people with insomnia have clinical depression, and up to 80% of patients with depression experience bouts of insomnia . Early wakening is closely associated with depression, as well as difficulty falling asleep at night. Those with depression may switch back and forth between insomnia and hypersomnia during a single period of depression.
Symptoms of Depression
In addition to troubling moods and thoughts, depression can also manifest in physical changes that interfere with daily activities. Symptoms may include :
- Persistent sad, low, or irritable mood
- Feelings of hopelessness, worthlessness, or guilt
- Loss of interest or pleasure in activities
- Decreased energy and fatigue
- Difficulty concentrating
- Insomnia, waking up too early, or oversleeping
- Low appetite or overeating
- Thoughts of death or suicide
Depression is more common in women, and there may be differences in the symptoms of depression based on sex and age. Men often experience symptoms such as anger, whereas women more frequently experience sadness and guilt. Adolescents with depression may be irritable and have trouble in school, and younger children may pretend to be sick to stay at home.
Seasonal affective disorder (SAD) is a type of depression that occurs at specific times of the year when there is less sunlight. In winter, less natural sunlight each day leads to more melatonin being released, which may trigger depression in some people. Someone who notices symptoms of depression only appear or worsen during certain seasons should speak to their doctor about targeted treatment options.
Treatments for Depression
Fortunately, people who undergo treatment for major depression often report improved sleep quality. After working with a doctor or mental health provider to understand the type and severity of depression, a treatment plan will be created accordingly.
- Counseling: Depression can be treated effectively with several types of counseling, including cognitive behavioral therapy (CBT) and interpersonal therapy (IPT). Cognitive behavioral therapy for insomnia (CBT-I) is a type of CBT that focuses on managing chronic insomnia.
- Medications: Antidepressants usually take time before they begin to improve symptoms and people may need to try several antidepressants at various doses before finding the right fit. A doctor or psychiatrist can discuss the appropriateness of these medications and recommend a specific type.
- Brain stimulation therapies: When medications and other approaches are not effective, some people with depression consider electroconvulsive therapy (ECT) or emerging methods of brain stimulation like repetitive transcranial magnetic stimulation (rTMS) and vagus nerve stimulation (VNS).
These approaches are often used in tandem to develop an effective treatment protocol. A combination of medication and psychotherapy has shown higher rates of improvement than one approach alone.
Tips for Sleeping Better With Depression
Sleep problems can increase the risk of initially developing depression, and persistent sleep issues can also increase the risk of relapse in people who have successfully been treated for depression. As a result, implementing these healthy habits can both help you sleep better, boost your mood, and help decrease some of the challenging symptoms of depression.
Talk to a Therapist
There are several different kinds of therapy to help you cope with depression and change your thought patterns around sleep. Therapeutic models such as CBT and psychotherapy can help you process some of the underlying feelings and challenges that contribute to depression. Mental health professionals can also suggest concrete behavioral changes to mitigate some of the symptoms of depression and provide coping mechanisms to manage restless nights.
Keep a Consistent Sleep Schedule
Suffering from depression can make it difficult to stick to a routine. Waking up and going to sleep at the same time each day gives your body an opportunity to get at least seven hours of sleep per night. Additionally, establishing a nightly routine provides a cue for the body to wind down and prime itself for sleep.
Nap Carefully
Restless or inconsistent sleep at night can make it tempting to nap during the day, but it is important to keep naps relatively brief. Research has found that a “power nap”, between 10 and 20 minutes, can help regulate emotions, reduce sleepiness, and lead to an overall uptick in performance. Naps that last longer than 20 minutes could interfere with your ability to fall asleep, while naps shorter than 10 minutes are not long enough to gain the benefits from napping.
Avoid Alcohol
It can be tempting to have a drink or two to promote relaxation and sleepiness, but alcohol has a harmful effect on sleep. While studies have shown that binge-drinking before bed leads to difficulty falling asleep and staying asleep, even moderate drinking is enough to disrupt the sleep cycle and shorten REM sleep.
Get Outside
Spending time outdoors is one of the simplest ways to aid your sleep if you suffer from depression. Exposure to sunlight aligns the body’s internal clock and circadian rhythms, giving cues for when to be alert and when to sleep. As the sun sets, the body then produces melatonin to induce sleepiness and promote sleep. Time outside can be a simple and effective way to trigger the natural chemicals in the brain that promote high-quality sleep.
Exercise Regularly
Research indicates those who engage in light, moderate, or vigorous exercise reported very good or fairly good sleep quality. Additionally, regular exercise has shown to significantly decrease symptoms of depression, making it an excellent choice to promote sleep health and mental health. If you decide to implement an exercise regimen, consider doing your workout during the first half of the day, as exercising in the evening could interfere with your ability to fall asleep.
When to Speak With Your Doctor
If your sleep quality or general quality of life is routinely affected by troubling feelings or low mood, it is important to share these concerns with a health care provider. Typically, symptoms must remain present for at least two weeks to be formally diagnosed as clinical depression. A medical professional can determine whether your symptoms are caused by depression or another health condition.
Frequently Asked Questions About Depression and Sleep
What Causes Depression?
While the exact cause of depression is unknown, there are a number of factors that can increase the risk of developing the condition. These include having a personal or familial history of depression, experiencing major stressors or traumas, taking certain medications, and having specific illnesses.
How is Depression Diagnosed?
Depression can only be diagnosed by a medical professional, so people experiencing symptoms of depression should speak with a doctor, counselor, or psychiatrist. They will likely ask about the severity and duration of your symptoms, and may conduct tests to determine the best course of treatment for your specific concerns.
Do Depressed People Need More Sleep?
Depression can cause fragmented sleep, which may lead to increased levels of sleepiness and fatigue during waking hours. Those who are experiencing difficult depression-related symptoms may feel the need to sleep more than usual, but most adults should aim to get at least seven hours of sleep per day.
Can Depression Lead to Sleep Disorders?
Depression has been linked to several sleep disorders, such as insomnia and obstructive sleep apnea. Since sleep and depression are often intertwined, it can be difficult to determine whether depression is the cause of one’s sleep problems, or if these sleep issues are a cause of depression.
Medical Disclaimer: The content on this page should not be taken as medical advice or used as a recommendation for any specific treatment or medication. Always consult your doctor before taking a new medication or changing your current treatment.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
7 Sources
-
Jindal, R. (2004). Treatment of insomnia associated with clinical depression. Sleep Medicine Reviews, 8(1), 19–30.
https://linkinghub.elsevier.com/retrieve/pii/S108707920300025X -
Franzen, P. L., & Buysse, D. J. (2008). Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues in clinical neuroscience, 10(4), 473–481.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108260/ -
Daut, R. A., & Fonken, L. K. (2019). Circadian regulation of depression: A role for serotonin. Frontiers in Neuroendocrinology, 54, 100746.
https://linkinghub.elsevier.com/retrieve/pii/S009130221930010X -
Meerlo, P., Sgoifo, A., & Suchecki, D. (2008). Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Medicine Reviews, 12(3), 197–210.
https://linkinghub.elsevier.com/retrieve/pii/S1087079207000986 -
Bonnet, M., & Arand, D. (2022, April 15). Risk factors, comorbidities, and consequences of insomnia in adults. In R. Benca (Ed.). UpToDate., Retrieved January 30, 2023, from
https://www.uptodate.com/contents/risk-factors-comorbidities-and-consequences-of-insomnia-in-adults -
Anxiety and Depression Association of America. (2023, January 18). Symptoms.
https://adaa.org/understanding-anxiety/depression/symptoms -
Consensus Conference Panel, Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., Dinges, D. F., Gangwisch, J., Grandner, M. A., Kushida, C., Malhotra, R. K., Martin, J. L., Patel, S. R., Quan, S. F., Tasali, E., Non-Participating Observers, Twery, M., Croft, J. B., Maher, E., … Heald, J. L. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Journal of Clinical Sleep Medicine, 11(6), 591–592.
https://pubmed.ncbi.nlm.nih.gov/25979105/
















