When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Dementia and Sleep
- People with dementia may experience increased daytime sleepiness and cognitive impairment.
- Loss of brain function disrupts the regulation of sleep-wake cycles.
- Dementia often changes sleep patterns, impacting both individuals with dementia and their caregivers.
- Behavioral strategies and a sleep routine may help manage sleep issues related to dementia.
Dementia is an irreversible loss of brain function that affects memory, language, problem-solving, and other cognitive processes. There are different types of dementia, all of which tend to affect older adults. Dementia is marked by brain cells not functioning as they should and dying off more quickly than they do in people without dementia. There isn’t a known cure for dementia, but available treatments can slow its progression.
Sleep problems are common in individuals with dementia, and sleep loss may contribute to or exacerbate the severity of other dementia symptoms. Caregivers report disturbed sleep to be one of the most distressing dementia symptoms. Identifying and treating sleep issues is a critical part of dementia care as it alleviates stress for patients and caregivers and could potentially slow cognitive decline.
Looking to improve your sleep? Try upgrading your mattress.
How Does Dementia Change Sleep Patterns?
Circadian rhythm is a collection of physical and psychological processes that guide our sleep-wake cycle by responding to indicators in our environment. People with dementia experience fundamental changes in their circadian rhythm that work against getting quality sleep on a regular schedule.
The suprachiasmatic nucleus (SCN) is the part of the brain that serves as our internal clock and responds to cues, such as light, to indicate when we should be alert and when we should feel sleepy. Individuals who have Alzheimer’s disease—the most common type of dementia—often have damaged cells in the SCN and decreased cellular activity in this part of the brain. The result of this dysfunction is that patients are often unable to follow a 24-hour sleep-wake cycle and instead sleep excessively during the day and sleep much less at night.
Additionally, dementia is associated with changes in sleep structure. When we sleep, our bodies cycle through a series of sleep stages, from light sleep (stages 1 and 2), to deep sleep (stage 3 or slow-wave sleep), and then dream sleep (also called rapid eye movement or REM sleep). Slow-wave sleep and REM sleep are critical parts of how sleep works to restore the body and mind. People with dementia spend less time in slow-wave sleep and REM sleep and more time in the earlier stages of sleep. This reduction of deep sleep and REM sleep can worsen as dementia progresses.
Normal Sleep Pattern Changes in Older Age
Research has documented a number of sleep changes that occur in healthy aging adults. These include bedtimes and wake times shifting to an earlier hour, taking longer to fall asleep once in bed, experiencing fragmented sleep, sleeping fewer hours per night, and spending less time in slow-wave and REM sleep. Although these changes parallel some of the sleep challenges seen in people with dementia, the sleep pattern changes in dementia patients tend to be more dramatic and disruptive.
Common Sleep Disorders in People With Dementia
People with dementia are frequently affected by sleep disorders. The following sleep disorders are found most often in older adults, but they are seen at even higher rates in people with dementia.
- Restless legs syndrome (RLS): RLS is characterized by an overwhelming desire to move the legs, especially at night. RLS is common in people with a type of dementia called Lewy body dementia.
- Periodic limb movement disorder (PLMD): PLMD causes uncontrollable movements of the arms and/or legs at night. Many patients with PLMD also have RLS.
- Obstructive sleep apnea (OSA): OSA is a condition marked by nighttime airway collapse leading to brief lapses in breathing. OSA is particularly common with Alzheimer’s disease, occurring in 40% of patients. Having OSA also increases one’s risk of developing dementia.
- REM sleep behavior disorder: REM sleep behavior disorder causes individuals to act out their dreams, sometimes in dangerous ways. It is most often found in individuals with Lewy body dementia and is sometimes the first symptom that arises with this type of dementia.
- Depression: Although depression is a mood disorder, it is associated with insomnia and other sleep disturbances. Depression is common in people with dementia, and it is seen at increasing rates as dementia progresses to more severe stages.
Other Sleep Issues in People With Dementia
“Sundowning” is a phenomenon in which individuals with dementia experience increased agitation later in the day and in the evening. The symptoms of sundowning include confusion, anxiety, wandering, and yelling. Sundowning can contribute to insomnia and other sleep problems when these behaviors continue into the night. Possible causes of sundowning include the circadian rhythm changes that occur in dementia, as well as fatigue, depression, and pain.
People with dementia may also talk, yell, or cry out at night if they cannot sleep. Some dementia patients have a tendency to wander away from their homes, which can be especially dangerous at night. In dementia patients with REM sleep behavior disorder, shouting, grabbing, jumping, and other behaviors are related to dream enactment during sleep.
How Does Sleep Affect Dementia Risk?
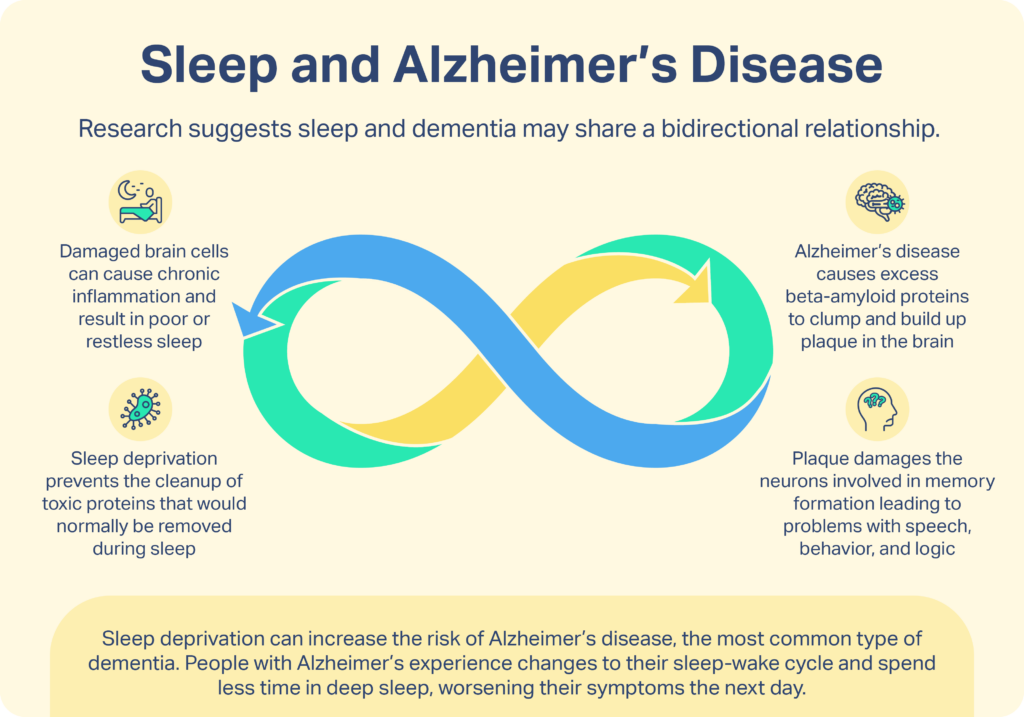
Experts suggest that sleep and dementia may share a bidirectional relationship. This means that while sleep could affect dementia risk and symptoms, the presence or absence of dementia also affects sleep quality. For example, one of the first Alzheimer’s disease symptoms in the brain is the accumulation of a protein called amyloid-beta, which eventually forms clumps called amyloid plaques. Animal studies and a small study in people have shown sleep deprivation to increase the levels of amyloid-beta in the brain. At the same time, Alzheimer’s patients with amyloid plaques have been shown to have worse sleep quality than Alzheimer’s patients who do not have amyloid plaques.
Additionally, sleep is known to be critical for our cognitive functioning and memory formation. Observational studies have shown that sleep issues are associated with cognitive decline and dementia. However, these studies do not prove a cause-and-effect relationship. Although more research is needed to better understand sleep and dementia risk, there are many proven steps you can take to improve your sleep.
What Can Help Someone With Dementia Sleep Better?
Sleep hygiene is the primary treatment for sleep concerns in people with dementia. Sleep hygiene is a collection of practices and environmental considerations that promote good sleep quality. The following sleep hygiene tips may help a person with dementia improve their sleep patterns:
- Maintain a regular schedule: Setting predictable wake and sleep times may help to synchronize circadian rhythm in people with dementia. Create a bedtime routine that involves quiet, soothing activities before bed. Television and electronic devices can be stimulating and emit blue light that interferes with sleep, so try avoiding these activities before bed.
- Limit naps: Napping during the day can decrease sleepiness at night, so it may help to discourage napping or limit the practice to one nap lasting less than 30 minutes.
- Engage in physical exercise: Exercising in the hour before bedtime can negatively affect sleep. However, getting exercise early in the day can lead to better sleep at night. It also reduces napping and supports overall health.
- Schedule social activity: A research study found that people with dementia who participated in one to two hours of social activity per day showed improved nighttime sleep.
- Add light exposure: Light is a key regulator of circadian rhythm, so if possible, getting natural light during the day can help with sleep at night. If access to natural light is limited due to weather or other factors, indoor bright light therapy may help.
- Avoid stimulants: It’s best to avoid caffeine, alcohol, and nicotine if possible. Additionally, some medications used to manage dementia can interfere with sleep, so talk with a doctor about the best time of day to administer medications.
- Treat pain and sleep disorders: If a person with dementia is dealing with pain, a sleep disorder, or depression, treating the condition may improve sleep. A doctor can help with exploring treatment options.
- Create a calming bedroom environment: A dark, quiet, comfortable bedroom promotes sleep. Some people with dementia benefit from having well-loved objects near their bed. If total darkness is not calming, add night lights to create a sense of security.
Some of these sleep hygiene practices may be difficult for someone with dementia. For example, it may not be possible to control the bedroom noise level in a nursing home or assisted living facility. Consider adding a white noise machine to mask outside noise. A person with dementia may also have a difficult time maintaining a regular bedtime due to napping or varied daily activities, but keeping wake time consistent can still help to stabilize the circadian rhythm. A physician or sleep specialist is in a good position to provide individualized sleep hygiene recommendations for a specific situation.
Medications for Dementia
Medications are seen as a last-resort option for people with dementia. The risks of sleep aids include increased confusion, sedation, and risk for falls or injury. Be sure to speak with a doctor before giving a sleep aid to a person with dementia.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
16 Sources
-
Rowe, M. A., Kelly, A., Horne, C., Lane, S., Campbell, J., Lehman, B., Phipps, C., Keller, M., & Benito, A. P. (2009). Reducing dangerous nighttime events in persons with dementia by using a nighttime monitoring system. Alzheimer’s & dementia : the journal of the Alzheimer’s Association, 5(5), 419–426.
https://pubmed.ncbi.nlm.nih.gov/19751921/ -
Petit, D., Gagnon, J. F., Fantini, M. L., Ferini-Strambi, L., & Montplaisir, J. (2004). Sleep and quantitative EEG in neurodegenerative disorders. Journal of psychosomatic research, 56(5), 487–496.
https://linkinghub.elsevier.com/retrieve/pii/S0022399904000182 -
Mander, B. A., Winer, J. R., & Walker, M. P. (2017). Sleep and Human Aging. Neuron, 94(1), 19–36.
https://pubmed.ncbi.nlm.nih.gov/28384471/ -
Ooms, S., & Ju, Y. E. (2016). Treatment of Sleep Disorders in Dementia. Current treatment options in neurology, 18(9), 40.
https://pubmed.ncbi.nlm.nih.gov/27476067/ -
MedlinePlus: National Library of Medicine (US). (2016, April 1). Lewy Body Dementia.
https://medlineplus.gov/lewybodydementia.html -
Suzuki, K., Miyamoto, M., & Hirata, K. (2017). Sleep disorders in the elderly: Diagnosis and management. Journal of General and Family Medicine, 18(2), 61–71.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5689397/ -
National Institute on Aging. (2017, May 17). Tips for Coping with Sundowning.
https://www.nia.nih.gov/health/tips-coping-sundowning -
National Institute on Aging. (2017, May 17). Wandering and Alzheimer’s Disease.
https://www.nia.nih.gov/health/wandering-and-alzheimers-disease -
Trotti L. M. (2010). REM sleep behaviour disorder in older individuals: epidemiology, pathophysiology and management. Drugs & aging, 27(6), 457–470.
https://pubmed.ncbi.nlm.nih.gov/20524706/ -
Ju, Y. E., Lucey, B. P., & Holtzman, D. M. (2014). Sleep and Alzheimer disease pathology–a bidirectional relationship. Nature reviews. Neurology, 10(2), 115–119.
https://pubmed.ncbi.nlm.nih.gov/24366271/ -
National Institutes of Health. (2018, April 13). Lack of sleep may be linked to risk factor for Alzheimer’s disease.
https://www.nih.gov/news-events/lack-sleep-may-be-linked-risk-factor-alzheimers-disease -
Spira, A. P., Chen-Edinboro, L. P., Wu, M. N., & Yaffe, K. (2014). Impact of sleep on the risk of cognitive decline and dementia. Current opinion in psychiatry, 27(6), 478–483.
https://pubmed.ncbi.nlm.nih.gov/25188896/ -
A.D.A.M. Medical Encyclopedia. (2020, April 25). Dementia – behavior and sleep problems.
https://medlineplus.gov/ency/patientinstructions/000029.htm -
Rose, K. M., & Lorenz, R. (2010). Sleep disturbances in dementia. Journal of gerontological nursing, 36(5), 9–14.
https://pubmed.ncbi.nlm.nih.gov/20438013/ -
National Institute on Aging. (2017, May 18). Staying Physically Active with Alzheimer’s.
https://www.nia.nih.gov/health/staying-physically-active-alzheimers -
Richards, K. C., Beck, C., O’Sullivan, P. S., & Shue, V. M. (2005). Effect of individualized social activity on sleep in nursing home residents with dementia. Journal of the American Geriatrics Society, 53(9), 1510–1517.
https://onlinelibrary.wiley.com/doi/10.1111/j.1532-5415.2005.53460.x
















