When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Insomnia and Women
The experience of lying in bed at night, sometimes for more than half an hour, and being unable to fall asleep can be particularly frustrating. So can long stretches of wakefulness in the night—or waking up well before your alarm clock is due to ring in the morning.
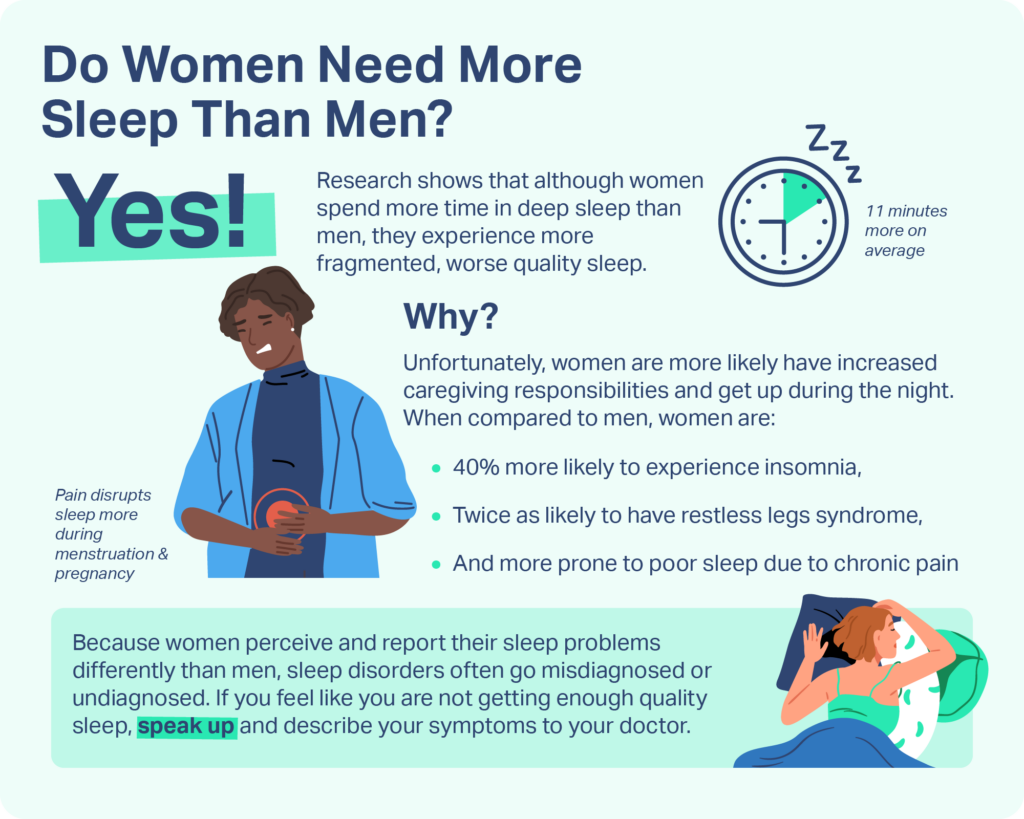
These symptoms are particularly common among women, who, by some estimates, are 40% more likely than men to experience insomnia during their lifetimes. Insomnia can negatively impact health and wellbeing, a person’s ability to perform daily tasks, and their relationships and quality of life. For these reasons, women should be aware of the risk factors for insomnia and steps they can take to get better sleep.
Struggling to Stay Awake? Take an At-Home Sleep Test

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
Is Insomnia More Common in Women?
In one recent survey, nearly a third of women reported that insomnia negatively affects their daily lives, versus about a quarter of men. Women are more likely to have trouble falling asleep and staying asleep than men, and they’re 1.8 times as likely as men to report that they rarely or never feel well-rested upon waking.
While more research on sleep disorders in transgender individuals is needed, limited evidence suggests strikingly high rates of insomnia symptoms both in trans women and trans men—though the causes of insomnia may differ between these groups.
What Causes Insomnia in Women?
There are many risk factors for and causes of insomnia in women and people assigned female at birth. Some biological processes, such as hormonal shifts, are associated with insomnia symptoms, as are a number of physical and mental health conditions. But external factors, including stressful life events and work and family demands, can also trigger insomnia. Additionally, some people experience long-term insomnia without an identifiable cause.
The Menstrual Cycle
People who menstruate are more likely to experience sleep problems at certain points during their cycles. Between ovulation and menstruation—roughly the last two weeks in a 28-day cycle—women are more likely to wake in the night and have trouble falling back asleep. This may be because of hormone-driven changes in sleep architecture, which reduce the amount of time women spend in deep sleep.
Insomnia symptoms are especially common among individuals with premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD), both of which cause physical discomfort and intense emotions in the leadup to menstruation. PMDD, in particular, is associated with decreased responsiveness to the sleep hormone melatonin and reductions in sleep duration during the weeks preceding a period.
Additionally, painful camps, heavy bleeding, and irregular periods can all contribute to poor sleep.
Pregnancy
Individuals also have an increased risk of developing insomnia during pregnancy, especially in the third trimester. Physical discomfort, acid reflux, the frequent need to urinate, and the baby’s movements can all contribute to an uptick in nighttime awakenings and difficulty falling asleep. Moreover, many people develop restless legs syndrome (RLS) or obstructive sleep apnea (OSA) during pregnancy, both of which increase their vulnerability to insomnia.
Pregnant people may also have trouble sleeping due to worries about the health of the baby, their own health, birth, or the looming changes in their lives. Unfortunately, insomnia that begins during pregnancy often persists in the postpartum period.
Menopause
Sleep problems become increasingly common in the years preceding and following menopause, which occurs twelve months after a person’s final menstrual period. Many factors can contribute to menopausal insomnia, including the experience of hot flashes—or night sweats. These events affect the vast majority of women during the menopausal transition. Physical discomfort, along with having to change soaked clothing and bedding, can lead to feelings of anxiety and irritation that make it even harder to fall back asleep.
The hormonal signals that govern sleeping and waking also weaken following menopause, which may contribute to sleep disturbances. Additionally, during and following the menopausal transition, individuals have an increased likelihood of developing conditions that have been linked to insomnia, including restless legs syndrome (RLS), sleep apnea, depression, and anxiety.
Stress and Mood Disorders
Evidence suggests that women are more likely than men to lose sleep as a result of stress, which makes them more vulnerable to insomnia. Moreover, women are disproportionately affected by certain mental health conditions that tend to co-occur with insomnia, including depression and anxiety. These disorders appear to have a bi-directional relationship with insomnia, meaning that depression and anxiety can lead to insomnia, and insomnia can aggravate the symptoms of depression and anxiety.
Women are especially likely to experience depression in the final stage of their menstrual cycle, during and after pregnancy, and in the leadup to menopause—so experts speculate that hormonal shifts can trigger depression. This may account for the increased prevalence of insomnia in these time periods.
Disrupted Sleep Schedules
To get healthy sleep, a person’s sleep schedule needs to align with their circadian rhythms, which are internal biological patterns that operate on a 24-hour clock. However, many women face pressures and responsibilities at home that prevent them from sleeping when their bodies tell them to.
Generally, females experience a rise in the sleep hormone melatonin earlier in the evening than males do, which means that women usually benefit from earlier bedtimes. However, some women may choose to stay up late in order to spend time with a “night owl” partner, which has the potential to create circadian misalignments that contribute to insomnia.
Moreover, research indicates that within households, women generally bear the bulk of responsibilities related to housework and caregiving. Staying up late to do chores—or getting up at night to care for children or ailing parents—can disrupt circadian rhythms and make it harder to sleep.
Pain
Pain can make it harder to sleep, and conversely, sleep difficulties can intensify pain and even cause new pain to develop. Research indicates that women are more likely than men to develop pain conditions, including:
- Migraines and tension headaches
- Carpal tunnel syndrome
- Irritable bowel syndrome
- Rheumatoid arthritis
- Fibromyalgia
Women, therefore, appear to be at greater risk of developing insomnia due to chronic pain.
Gender Affirming Hormone Therapy
Gender affirming hormone therapy appears to have a negative impact on sleep for both trans men and trans women. Trans men may be particularly susceptible to insomnia. Testosterone therapy may induce sleep disordered breathing in trans men. And regardless of whether or not they use hormone therapy, trans men are more likely to have hot flashes or night sweats that disturb their sleep.
How Can Women Get Better Sleep?
Short-term insomnia can often be resolved by identifying and addressing its root causes. There are several steps you can take to limit the impacts of physical and mental stressors on your sleep.
- Keep a regular sleep schedule. Committing to a consistent bedtime that aligns with your circadian rhythms can help you sleep better.
- Try relaxation techniques. Consider integrating practices that reduce stress into your bedtime routine. Try reflective journaling, meditation, or gentle yoga.
- Ask for help. If possible, ask your partner or a family member to help with caregiving and household responsibilities—especially those that interfere with sleep.
- Prioritize your health. Eating a nutritious diet and getting regular exercise can help improve sleep, alleviate the symptoms of PMS and menopause, manage depression, and even reduce chronic pain.
If these steps don’t help, or if your insomnia persists beyond a few weeks, you should talk to a medical professional about your concerns. Depending on the sources of your sleep difficulties, your doctor might recommend one or more treatment options, such as cognitive behavioral therapy for insomnia (CBT-I), mental health counseling, menopausal hormone therapy, melatonin supplements, or antidepressant medication.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
16 Sources
-
American Academy of Sleep Medicine. (2022, June). AASM Sleep Prioritization Survey, Insomnia Impact on Daily Life.
https://aasm.org/wp-content/uploads/2022/06/sleep-prioritization-survey-insomnia-impact.pdf -
Adjaye-Gbewonyo, D., Ng, A., & Black, L. (2022, June). Sleep Difficulties in Adults: United States, 2020. National Center for Health Statistics.
https://www.cdc.gov/nchs/products/databriefs/db436.htm -
Auer, M. K., Liedl, A., Fuss, J., Nieder, T., Briken, P., Stalla, G. K., Hildebrandt, T., Biedermann, S. V., & Sievers, C. (2017). High impact of sleeping problems on quality of life in transgender individuals: A cross-sectional multicenter study. PloS one, 12(2), e0171640.
https://pubmed.ncbi.nlm.nih.gov/28199359 -
Neubauer, D., Bonnet, M., & Arand, D. (2024, February). Evaluation and diagnosis of insomnia in adults. In R. Benca & A. Eichler (Ed.). UpToDate.
https://www.uptodate.com/contents/evaluation-and-diagnosis-of-insomnia-in-adults -
Jehan, S., Auguste, E., Hussain, M., Pandi-Perumal, S. R., Brzezinski, A., Gupta, R., Attarian, H., Jean-Louis, G., & McFarlane, S. I. (2016). Sleep and Premenstrual Syndrome. Journal of sleep medicine and disorders, 3(5), 1061.
https://pubmed.ncbi.nlm.nih.gov/28239684/ -
Mong, J. A., & Cusmano, D. M. (2016). Sex differences in sleep: impact of biological sex and sex steroids. Philosophical transactions of the Royal Society of London. Series B, Biological sciences, 371(1688), 20150110.
https://pubmed.ncbi.nlm.nih.gov/26833831/ -
Jeon, B., & Baek, J. (2023). Menstrual disturbances and its association with sleep disturbances: a systematic review. BMC women’s health, 23(1), 470.
https://pubmed.ncbi.nlm.nih.gov/37658359/ -
Silvestri, R., & Aricò, I. (2019). Sleep disorders in pregnancy. Sleep science (Sao Paulo, Brazil), 12(3), 232–239.
https://pubmed.ncbi.nlm.nih.gov/31890101/ -
Gallaher, K. G. H., Slyepchenko, A., Frey, B. N., Urstad, K., & Dørheim, S. K. (2018). The Role of Circadian Rhythms in Postpartum Sleep and Mood. Sleep medicine clinics, 13(3), 359–374.
https://pubmed.ncbi.nlm.nih.gov/30098753/ -
Pérez-Medina-Carballo, R., Kosmadopoulos, A., Boudreau, P., Robert, M., Walker, C. D., & Boivin, D. B. (2023). The circadian variation of sleep and alertness of postmenopausal women. Sleep, 46(2), zsac272.
https://pubmed.ncbi.nlm.nih.gov/36420995 -
Casper, R. (2024, February). Clinical manifestations and diagnosis of menopause. In R. Barbieri, W. Crowley, & K. Martin (Ed.). UpToDate.
https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-menopause -
Barsha, R. A. A., & Hossain, M. B. (2020). Trouble Sleeping and Depression Among US Women Aged 20 to 30 Years. Preventing chronic disease, 17, E29.
https://pubmed.ncbi.nlm.nih.gov/32242798 -
Spitschan, M., Santhi, N., Ahluwalia, A., Fischer, D., Hunt, L., Karp, N. A., Lévi, F., Pineda-Torra, I., Vidafar, P., & White, R. (2022). Sex differences and sex bias in human circadian and sleep physiology research.
https://pubmed.ncbi.nlm.nih.gov/35179486 -
Casale, R., Atzeni, F., Bazzichi, L., Beretta, G., Costantini, E., Sacerdote, P., & Tassorelli, C. (2021). Pain in Women: A Perspective Review on a Relevant Clinical Issue that Deserves Prioritization. Pain and therapy, 10(1), 287–314.
https://pubmed.ncbi.nlm.nih.gov/33723717 -
Hershner, S., Jansen, E. C., Gavidia, R., Matlen, L., Hoban, M., & Dunietz, G. L. (2021). Associations Between Transgender Identity, Sleep, Mental Health and Suicidality Among a North American Cohort of College Students. Nature and science of sleep, 13, 383–398.
https://pubmed.ncbi.nlm.nih.gov/33762860/ -
Auer, M. K., Liedl, A., Fuss, J., Nieder, T., Briken, P., Stalla, G. K., Hildebrandt, T., Biedermann, S. V., & Sievers, C. (2017). High impact of sleeping problems on quality of life in transgender individuals: A cross-sectional multicenter study. PloS one, 12(2), e0171640.
https://pubmed.ncbi.nlm.nih.gov/28199359/