When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
How Sleep Deprivation Affects Your Heart
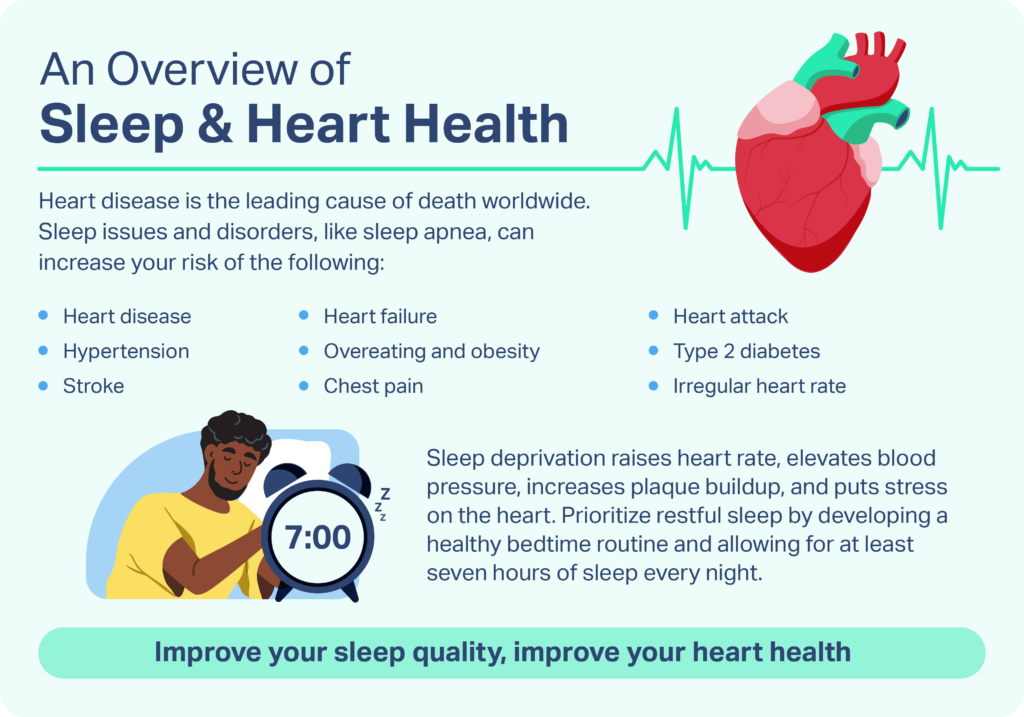
- Lack of sleep can impair metabolism, cause inflammation, raise blood pressure, and increase your risk of cardiovascular diseases.
- Sleep disorders, like sleep apnea, disrupt sleep and decrease oxygen levels, leading to heart rhythm irregularities and stress.
- Exercise, meditation, and other behavioral changes can lessen your risk for both sleep deprivation and heart problems.
It’s difficult to overstate the heart’s importance to health. Responsible for pumping blood throughout the body, the heart powers the circulatory system that ensures that all the organs and tissues in the body get the oxygen they need.
Unfortunately, heart problems are a leading cause of illness and death in the United States. While it’s already well-known that factors like poor diet, limited exercise, and smoking can harm the heart, there’s a growing recognition of the dangers of sleep deprivation for heart health.
Sleep provides time for the body to restore and recharge, playing a key role in nearly all aspects of physical health. As a result, getting good sleep may help prevent damage to the cardiovascular system, and for people with heart problems, can be part of following a heart-healthy lifestyle.
Looking to improve your sleep? Try upgrading your mattress.
Does Sleep Deprivation Affect Heart Health?
Substantial evidence demonstrates that sleeping problems, including sleep deprivation and fragmented sleep, have negative effects on heart health.
Sleep is an essential time for the body to recuperate. During the non-rapid eye movement (NREM) sleep stages, heart rate slows, blood pressure drops, and breathing stabilizes. These changes reduce stress on the heart, allowing it to recover from strain that occurs during waking hours.
Without sufficient nightly sleep, a person doesn’t spend enough time in the deep stages of NREM sleep that benefit the heart. The same problem can affect people whose sleep is frequently interrupted. Chronic sleep deprivation has been linked to numerous heart problems including high blood pressure, high cholesterol, heart attack, obesity, diabetes, and stroke.
Sleep and Blood Pressure
During normal, healthy sleep, blood pressure drops by around 10-20%. This is known as nocturnal dipping, and research highlights its role in cardiovascular health. Non-dipping has been tied to an increased risk of stroke, heart attack, kidney problems, and reduced blood flow to the brain.
Studies have also found that elevated nighttime blood pressure is tied to overall high blood pressure (hypertension). In fact, nocturnal blood pressure has been found to be even more predictive of heart problems than high blood pressure during the day.
Raised daytime blood pressure has been identified as a consequence of sleep deprivation in multiple studies, but it doesn’t affect all people equally. The link between lack of sleep and high blood pressure is highest in middle-aged adults. People who work long hours in high-stress jobs and people with other risk factors for hypertension are more likely to have raised blood pressure after chronic poor sleep.
Sleep and Coronary Heart Disease
Coronary heart disease is the leading cause of death in the United States. Also known as coronary artery disease, it happens when plaque builds up in the arteries, hardening and narrowing them in a condition known as atherosclerosis. This reduces the ability of the heart to get enough blood and oxygen.
Research has found that sleep deprivation contributes to atherosclerosis. Plaque forms as a consequence of inflammation, which involves white blood cells, which are produced by the immune system, to collect in the arteries. Poor sleep triggers chronic inflammation, which contributes to plaque formation and hardening of the arteries.
Sleep and Heart Failure
Heart failure is when the heart doesn’t pump enough blood to supply the body with the blood and oxygen that it needs to function properly. An observational study of over 400,000 people found strong associations between sleeping problems and heart failure.
In that study, people who slept less than seven hours per night had an elevated risk of heart failure. Heart failure was also more common in people who had other indicators of unhealthy sleep including insomnia symptoms, daytime sleepiness, snoring, and being an evening person. The more of these signs of unhealthy sleep that one person had, the higher their likelihood of heart failure.
Sleep and Heart Attacks
A heart attack, also known as myocardial infarction, happens when the flow of blood to the heart gets blocked. Sleep deprivation heightens the risk of heart attacks.
In one study, people sleeping less than six hours per night had a 20% higher chance of a heart attack. Sleep interruptions have also been linked to the potential for heart attacks. Because both heart rate and blood pressure can abruptly spike upon awakening, fragmented sleep can cause cardiac stress and may induce a heart attack.
Sleep and Stroke
A stroke is when blood flow to the brain is cut off, causing brain cells to die from lack of oxygen. Ischemic strokes occur when a blood clot or plaque blocks an artery. A transient ischemic attack (TIA), also referred to as a mini-stroke, involves only a short-term blockage.
In research studies, lack of sleep has been correlated with a greater likelihood of having a stroke. Sleep deprivation increases blood pressure, and high blood pressure is considered to be the leading risk factor for strokes. In addition, by contributing to plaque buildup in the arteries, insufficient sleep may make it easier for blockages to occur and cause mini-strokes or strokes.
Sleep and Obesity
Being overweight or obese is strongly associated with numerous cardiovascular and metabolic problems including hypertension, diabetes, high cholesterol, heart disease, heart attack, and stroke.
Lack of sleep is associated with obesity, whereby people who sleep less than seven hours per night are more likely to have a higher body mass index (BMI) or be obese. Sleep helps regulate the hormones that control hunger, and lack of sleep or sleep disturbances can trigger overeating and boost the desire for high-calorie foods.
Sleep and Type 2 Diabetes
Type 2 diabetes is a chronic condition in which the level of blood sugar, also known as blood glucose, is too high due to the body’s inability to process sugar properly. Excess blood glucose damages blood vessels, negatively affecting cardiovascular health. People with diabetes are twice as likely to die from heart disease or stroke than people without this condition.
Many factors affect blood sugar, but studies have found that a lack of sleep worsens glucose metabolism. Poor sleep is associated with prediabetes, a type of glucose intolerance that does not meet the parameters for diabetes. People already diagnosed with diabetes who have insufficient or restless sleep may have a harder time controlling their blood sugar. Impaired sleep may also worsen the hardening of arteries in people with type 2 diabetes.
Sleep and Heart Rate
In normal sleep, the heart rate drops during the NREM sleep stages and then picks back up as you prepare to wake up. Poor sleep, including abrupt awakenings, can generate a sharp uptick in heart rate. Research has also found that people with sleeping problems are more likely to complain of an irregular heartbeat. For these reasons, lack of sleep may be tied to heart palpitations.
In addition, a study in older adults found that people who have frequent nightmares were considerably more likely to report having an irregular heartbeat. Nightmares may increase heart rate, and if a person’s sleep is disturbed by a nightmare, they may wake up feeling like their heart is racing.
Sleep and Chest Pain
Angina is chest pain related to poor flow of blood through blood vessels. When sleep is interrupted, a quick surge in heart rate and blood pressure can cause angina, and studies have found an association between unexplained chest pain and poor sleep. While this connection isn’t fully understood, it may be related to stress and anxiety, which are emotional states more common in people who have poor sleep
Non-cardiac chest pain can be tied to sleep as well. People with heartburn and acid reflux often suffer from sleep disruptions, which may heighten their risk of experiencing an overlap between poor sleep and pain in their chest.
Sleep Disorders and Heart Health
Many sleep disorders have detrimental effects on heart health. Insomnia, one of the most common sleep disorders, is often accompanied by insufficient sleep and can lead to elevated cardiovascular health risks.
Obstructive sleep apnea (OSA) is a breathing disorder that is linked to heart disease, obesity, diabetes, stroke, and high blood pressure. People with OSA have lapses in breathing during sleep when their airway gets obstructed. In addition to restless sleep, disturbed respiration reduces the amount of oxygen in the blood, which may worsen the impacts of OSA on heart health.
Disorders of abnormal movement during sleep, such as restless leg syndrome and periodic limb movement disorder, have also been linked to heart problems. While the exact explanation is unknown, it may relate to abnormal activation of the cardiovascular system that occurs with these conditions and induces elevated and fluctuating heart rate and blood pressure.
Circadian rhythm sleep disorders, which occur when a person’s internal clock is misaligned with day and night, have been associated with cardiovascular problems. For example, people who work night shifts and have to sleep during the day have heightened risks of hypertension, obesity, and diabetes as well as cardiac events like a stroke or heart attack.
Sleep and Heart Health During Pregnancy
Pregnancy places additional strain on the heart and some women develop cardiovascular problems during pregnancy. High blood pressure, for example, can begin or worsen during pregnancy with potential complications for both the mother and her baby.
Insomnia, sleep apnea, and other sleep difficulties affect many pregnant women, and these issues have been associated with a higher risk of cardiovascular problems both during and after pregnancy. Ongoing research studies are working to identify ways to improve sleep during pregnancy with the goal of also reducing hypertension and other cardiovascular issues.
Sleeping Too Much and Heart Health
The impacts of sleep deprivation on heart health receive considerable attention, but many studies have also found associations between sleeping too much, generally defined as more than nine hours per night, and cardiovascular problems.
While more research is needed, many experts believe that underlying health conditions that cause excess sleep are also the cause of this higher rate of heart issues. Nevertheless, this data is a reminder that it’s a myth that more sleep is always better.
Sleep Tips for People With Heart Problems
Because sleep deprivation can harm the heart, it’s important for people with cardiovascular problems to make getting good sleep a priority. Some evidence even indicates that improving sleep may reduce the likelihood of heart attacks or other cardiovascular problems in people who are otherwise at high risk.
Unfortunately, some heart problems can interfere with sleep. For example, diabetes can cause frequent nighttime urination, and other cardiovascular disorders may create chest discomfort when trying to get to sleep. Worry and anxiety about heart health can also make it hard to wind down and fall asleep normally.
Because numerous factors can influence both sleep and cardiovascular health, it’s most helpful to talk with your doctor about heart-healthy sleep. A doctor can help develop a specific plan to improve your sleep and address other lifestyle factors that are important for your heart and overall wellness.
While there’s no silver bullet solution, certain tips can often help people with heart problems get better sleep.
- Develop strategies for relaxation: If heart concerns spur anxiety, they can keep your mind racing when you just want to ease into sleep. Techniques like deep breathing, yoga, light stretching, and mindfulness meditation are just a few beneficial approaches for people struggling with how to sleep with pericarditis (inflammation around the heart), heart disease, or other heart problems that cause chest pain.
- Plan a consistent sleep schedule: Keeping the same bedtime and wake-up time every day is widely considered to be one of the key ways to encourage healthy and stable sleep from night to night.
- Design an accommodating bedroom: Set your sleep environment to meet your needs by ensuring that the bedroom has a comfortable mattress and pillow, a pleasant temperature, and as much quiet and darkness as possible.
- Avoid negative influences on sleep: Alcohol and caffeine can both interfere with sleep and are best avoided at night. Excessive use of electronic devices, including your cell phone, can also throw off your sleep patterns, which is why experts recommend not using these devices for an hour or more before bed.
These tips and other elements of sleep hygiene can serve as a foundation for better sleep, creating habits that make it easier to get both the quantity and quality of sleep that you need.
Does Sleeping Position Affect Heart Health?
There is limited evidence linking a person’s sleeping position with their overall heart health. Some research that focuses on people with congestive heart failure has found that sleeping on your left side may change aspects of heart and lung function.
Congestive heart failure is a buildup of fluid in the lungs or other parts of the body that occurs when the heart isn’t pumping blood effectively. Studies have found that people with congestive heart failure frequently avoid sleeping on their left side. While the exact reason for this is unknown, it may relate to how this sleeping posture alters positioning of the heart, pressure on the lungs, and/or the sensation of the heart beating against the chest wall.
However, evidence has not shown that this sleeping position causes heart problems. Based on research to date, a person’s sleeping position is not considered to be a risk factor for heart disease or other cardiovascular problems.
References
17 Sources
-
Grandner, M. A., Alfonso-Miller, P., Fernandez-Mendoza, J., Shetty, S., Shenoy, S., & Combs, D. (2016). Sleep: important considerations for the prevention of cardiovascular disease. Current opinion in cardiology, 31(5), 551–565.
https://journals.lww.com/co-cardiology/Abstract/2016/09000/Sleep__important_considerations_for_the_prevention.12.aspx -
Calhoun, D. A., & Harding, S. M. (2010). Sleep and hypertension. Chest, 138(2), 434–443.
https://pubmed.ncbi.nlm.nih.gov/20682533/ -
Kuetting, D., Feisst, A., Sprinkart, A. M., Homsi, R., Luetkens, J., Thomas, D., Schild, H. H., & Dabir, D. (2019). Effects of a 24-hr-shift-related short-term sleep deprivation on cardiac function: A cardiac magnetic resonance-based study. Journal of sleep research, 28(3), e12665.
https://onlinelibrary.wiley.com/doi/10.1111/jsr.12665 -
National Institutes of Health (NIH). (2019, March 5). How disrupted sleep may lead to heart disease., Retrieved November 30, 2020, from
https://www.nih.gov/news-events/nih-research-matters/how-disrupted-sleep-may-lead-heart-disease -
Besedovsky, L., Lange, T., & Haack, M. (2019). The sleep-immune crosstalk in health and disease. Physiological Reviews, 99(3), 1325–1380.
https://journals.physiology.org/doi/full/10.1152/physrev.00010.2018 -
Li, X., Xue, Q., Wang, M., Zhou, T., Ma, H., Heianza, Y., & Qi, L. (2020). Adherence to a Healthy Sleep Pattern and Incident Heart Failure: A Prospective Study of 408802 UK Biobank Participants. Circulation, 10.1161/CIRCULATIONAHA.120.050792. Advance online publication.
https://pubmed.ncbi.nlm.nih.gov/33190528/ -
Daghlas, I., Dashti, H. S., Lane, J., Aragam, K. G., Rutter, M. K., Saxena, R., & Vetter, C. (2019). Sleep duration and myocardial infarction. Journal of the American College of Cardiology, 74(10), 1304–1314.
https://pubmed.ncbi.nlm.nih.gov/31488267/ -
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2017, February). Diabetes, Heart Disease, and Stroke.
https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/heart-disease-stroke -
Spiegel, K., Tasali, E., Leproult, R., & Van Cauter, E. (2009). Effects of poor and short sleep on glucose metabolism and obesity risk. Nature reviews. Endocrinology, 5(5), 253–261.
https://www.nature.com/articles/nrendo.2009.23 -
Yoda, K., Inaba, M., Hamamoto, K., Yoda, M., Tsuda, A., Mori, K., Imanishi, Y., Emoto, M., & Yamada, S. (2015). Association between poor glycemic control, impaired sleep quality, and increased arterial thickening in type 2 diabetic patients. PloS one, 10(4), e0122521.
https://pubmed.ncbi.nlm.nih.gov/25875738/ -
Asplund, R., & Aberg, H. (1998). Sleep and cardiac symptoms amongst women aged 40-64 years. Journal of internal medicine, 243(3), 209–213.
http://doi.wiley.com/10.1046/j.1365-2796.1998.00276.x -
Asplund R. (2003). Nightmares, sleep and cardiac symptoms in the elderly. The Netherlands journal of medicine, 61(7), 257–261.
https://pubmed.ncbi.nlm.nih.gov/14567523/ -
Jerlock, M., Kjellgren, K. I., Gaston-Johansson, F., Lissner, L., Manhem, K., Rosengren, A., & Welin, C. (2008). Psychosocial profile in men and women with unexplained chest pain. Journal of internal medicine, 264(3), 265–274.
https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2796.2008.01961.x -
National Heart, Lung, and Blood Institute (NHLBI). (2019, September 13). Pregnant women with sleep problems could face a lifetime of cardiovascular woes., Retrieved November 30, 2020, from
https://www.nhlbi.nih.gov/news/2019/pregnant-women-sleep-problems-could-face-lifetime-cardiovascular-woes -
Montano, N., Fiorelli, E., & Tobaldini, E. (2019). Sleep Duration and the Heart: I Sleep, Therefore I Beat. Journal of the American College of Cardiology, 74(10), 1315–1316.
https://linkinghub.elsevier.com/retrieve/pii/S0735109719360905 -
Bayraktar, M. F., & Ozeke, O. (2018). Serial echocardiographic changes with different body positions and sleeping side preference in heart failure patients. Echocardiography (Mount Kisco, N.Y.), 35(8), 1132–1137.
https://onlinelibrary.wiley.com/doi/10.1111/echo.13888 -
Leung, R. S., Bowman, M. E., Parker, J. D., Newton, G. E., & Bradley, T. D. (2003). Avoidance of the left lateral decubitus position during sleep in patients with heart failure: relationship to cardiac size and function. Journal of the American College of Cardiology, 41(2), 227–230.
https://linkinghub.elsevier.com/retrieve/pii/S0735109702027171












