When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Night Sweats in Women
- Definition: Night sweats are episodes of excessive sweating during sleep that can soak clothing or bedding.
- Causes: In women, night sweats are often linked to hormonal changes such as perimenopause, menopause, pregnancy, or postpartum, but can also be caused by stress or anxiety, infections, medications like antidepressants, or underlying health conditions like sleep apnea or acid reflux.
- Treatment: Reduce night sweats by addressing the underlying cause, investing in breathable bedding materials, cooling down your bedroom, and relieving stress before bed.
- When to talk to a doctor: If you experience other symptoms, like weight loss, fever, or fatigue, alongside night sweats, consult your healthcare provider.
Waking up sweaty despite a cool room can be alarming, and for many women, it’s a common experience. Night sweats can also be uncomfortable and disturb sleep, as some people sweat enough to soak through their pajamas and bedding.
Although many people have woken up sweaty due to heavy blankets, night sweats are not caused by the bedroom environment. Instead, the cause is internal. And while night sweats don’t necessarily mean there’s something medically wrong, their association with some serious conditions means it’s important to speak to your doctor if you’re concerned. Understanding the root of night sweats can also help you find the right treatment and improve the quality of your sleep.
Looking to improve your sleep? Try upgrading your mattress.
Overview of Night Sweats in Women
Night sweats refer to episodes of excessive sweating that occur during sleep, often soaking through clothes or bedding, even when the room is cool. And they’re a common complaint. In one study, 41% percent of people reported recently experiencing night sweats, but women tend to experience them more than men .
Part of the reason for this difference is that night sweats tend to accompany perimenopause and menopause. Still, there are many other physiological processes and underlying health conditions that can cause night sweats in men and women.
Common Causes of Night Sweats in Women
While sweating might seem like a simple reaction to heat or exercise, it’s a complex system influenced by many factors. Because of this, there’s no single answer to explain what causes night sweats in women. However, night sweats are often caused when a bodily process or underlying health condition impacts the thermoneutral zone.
The thermoneutral zone is the range of temperatures our body is comfortable with. While most people have a similar thermoneutral zone, it’s a dynamic range that can be influenced by gender, health, and fitness. If your thermoneutral zone increases or narrows during sleep, this change can provoke night sweats.
To understand why this happens, it’s important to look at the various causes—many of which are specific to women’s hormonal and physiological changes.
Perimenopause and Menopause
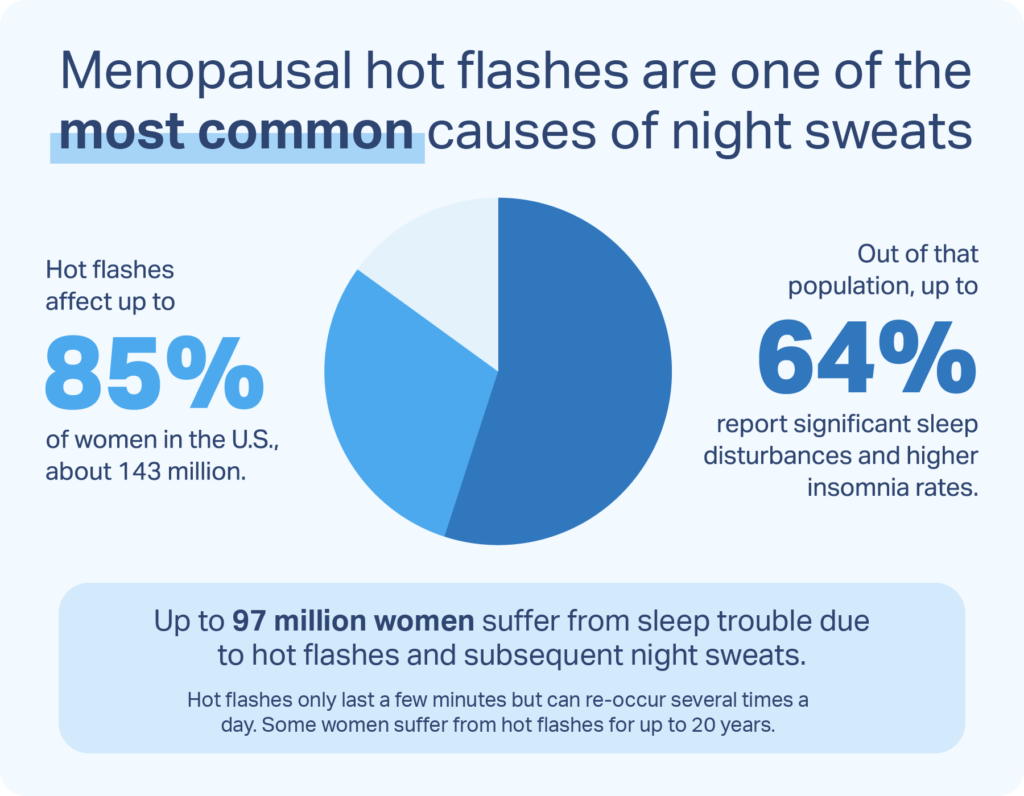
Hormones affect how we sweat. Up to 80% of women who are going through perimenopause or menopause experience hot flashes or night sweats. Together, these two symptoms are known as vasomotor menopausal symptoms and can cause discomfort and a lower quality of life for women who experience them.
Vasomotor menopausal symptoms can begin in perimenopause, the period of time before menopause that’s characterized by fluctuating hormones. In addition to continuing throughout menopause, vasomotor menopausal symptoms can also reoccur for post-menopausal women.
Signs that you may be entering perimenopause or menopause include:
- Changes to your menstrual cycle
- Vaginal dryness or infections
- Bladder incontinence or infections
- Difficulty sleeping
- Changes to your libido
- Mood disturbances
- Physical changes, including weight gain or loss
The severity of vasomotor menopausal symptoms can vary dramatically from person to person and within the same person over time. In addition to excessive and sometimes extreme sweating, menopause-related night sweats or hot flashes are often accompanied by red skin blotches, excessive sweating, and shivering. They usually last between 30 seconds and 10 minutes, though their frequency can range from multiple times an hour to multiple times a month.
Your doctor can provide additional information and support if you believe you may be going through perimenopause or menopause. While these life stages are a normal part of the aging process, there are treatments that can help alleviate symptoms like night sweats. Depending on the severity of your symptoms and other factors, these treatments may include lifestyle changes, dietary supplements, and hormonal or non-hormonal medication.
Menstruation, PMS, and PMDD
Some women experience night sweats at different stages of their menstrual cycle, often due to hormonal fluctuations that impact body temperature regulation. In the days leading up to menstruation, a drop in progesterone and estrogen levels can narrow the body’s thermoneutral zone, increasing the likelihood of nighttime sweating—even in a cool room.
Women with premenstrual syndrome (PMS) may also notice night sweats as part of a broader set of symptoms that include irritability, bloating, and fatigue. For those with premenstrual dysphoric disorder (PMDD), a more severe form of PMS, the effects can be even more disruptive.
These hormonal changes interfere with how the brain regulates core body temperature. As a result, the body may respond to subtle changes with exaggerated heat loss mechanisms, like sweating at night. Tracking symptoms alongside the menstrual cycle can help identify patterns and guide treatment options.
Pregnancy and Postpartum
Night sweats are a common experience during both pregnancy and the postpartum period. Research shows that over one-third of pregnant women report experiencing hot flashes or night sweats, with around 29% continuing to experience them after giving birth . These symptoms are most intense during the third trimester, particularly around week 30, and often peak again around two weeks postpartum.
The underlying cause is largely hormonal. During pregnancy, the body undergoes significant fluctuations in estrogen and progesterone, which can disrupt thermoregulation—the process by which the body maintains a stable internal temperature. This disruption often narrows the thermoneutral zone, making pregnant women more sensitive to small increases in core temperature and more likely to sweat at night as a result.
After delivery, the body rapidly shifts hormone levels once again as it transitions into lactation and postpartum recovery. This sudden drop, particularly in estrogen, may trigger excessive sweating, especially during sleep. In fact, postpartum night sweats are one of the body’s natural methods for shedding excess fluid accumulated during pregnancy.
While night sweats during this time are often normal, persistent or severe symptoms may warrant discussion with a doctor, especially if accompanied by fever, chills, or signs of hormonal imbalance.
Premature Ovarian Insufficiency
Premature ovarian insufficiency can cause some women to develop menopausal symptoms, including night sweats and hot flashes, at a much earlier age than would be explained by perimenopause.
Previously called ovarian failure, premature ovarian insufficiency occurs when the ovaries stop working normally before the age of 40, causing menopausal symptoms and fertility loss. It’s distinct from premature menopause, as women with premature ovarian insufficiency may still have occasional periods.
Researchers are still trying to understand what triggers premature ovarian insufficiency, and 90% of cases have an unknown cause. The condition is under-diagnosed and can increase a woman’s risk of infertility, osteoporosis, and heart disease, so it’s important to speak to your doctor if you experience any concerning symptoms. Premature ovarian insufficiency is a chronic condition, but there are treatments that can help alleviate uncomfortable symptoms like night sweats.
Anxiety and Stress
More than 30% of women are diagnosed with an anxiety disorder at some point in their lives, and around 63% of women report at least moderate stress levels. Both short-term and chronic anxiety or stress can cause night sweats, possibly by making sweat glands more responsive.
There’s also the possibility that anxiety may make people more likely to notice nighttime sweating, either due to anxiety-related sleep disturbances or because they’re worried about the health implications of night sweats. If you’re concerned about night sweats or your stress levels, your doctor can determine if you have any underlying health conditions and suggest treatment options.
Medications
Night sweats can be caused by medication you’re taking. Some people only experience night sweats, but other people find that their medication causes excessive sweating during the day as well. Some medications with this side effect include:
- Antidepressants, including tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs)
- Hormone replacement therapy, particularly treatments that affect estrogen or testosterone levels
- Painkillers like aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen
- Cortisone and some other corticosteroids
- Diabetes treatments like hypoglycemic agents
If you believe that your night sweats are caused by a medication you have been prescribed, talk to your doctor before you change your dosage or stop taking it.
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea (OSA) is a common sleep breathing disorder that can cause night sweats in some people. People with OSA experience multiple apneas, or pauses in their breathing, while asleep due to their airway collapsing or being blocked by excess tissue.
A reported 33% percent of women with OSA may experience night sweats due to the condition. However, sleep apnea treatment appears to help relieve this symptom. Other common symptoms of OSA include:
- Snoring, gasping, and choking during sleep
- Excessive daytime sleepiness
- Depression and other mood changes
- Difficulty concentrating during the day
- Regularly waking up during the night
OSA is a chronic condition that requires treatment. The most common treatment involves using a continuous positive airway pressure (CPAP) device, but other treatment options include lifestyle changes, oral appliances to open the airway, and surgery.
Infections
Infections release inflammatory mediators that raise your thermoneutral zone. This causes a familiar fever cycle, beginning with shivering to raise your internal temperature. Once your thermoneutral zone returns to normal, you will likely start sweating to decrease your temperature. This cycle usually occurs repeatedly during an infection and can cause night sweats if it happens at night. Your body’s viral or bacterial load may also rise during sleep, increasing the likelihood of night sweats.
Serious infections that can cause night sweats include:
- Tuberculosis, a bacterial lung infection
- Human immunodeficiency virus (HIV), a virus that attacks the body’s immune system
- Brucellosis, a bacterial infection transmitted from animals to humans, often through unpasteurized dairy or contact with infected animals
- Endocarditis, an infection of the inner lining of the heart chambers or valves (endocardium)
Hyperhidrosis
People with hyperhidrosis sweat excessively without being triggered by heat or exercise . The sweating can occur during the day or at night, and it can be severe enough to soak through clothing and bedding. Skin problems, particularly on the palms, can also develop due to excess moisture.
Hyperhidrosis can occur without an underlying trigger, or it can be caused by medication or a health condition. The most common treatments for this condition include oral and topical medication, surgery, and the use of botulinum toxin to block neurotransmitters.
Hyperthyroidism
Both night sweats and excessive daytime sweating are symptoms of hyperthyroidism, which is also known as having an overactive thyroid. Other symptoms of this common condition include weight loss, tremors, fatigue, heart palpitations, disturbed sleep, and anxiety. Night sweats and other symptoms usually respond well to treatment, which may include medications, radioactive iodine therapy, or, in some cases, surgery.
Gastroesophageal Reflux Disease (GERD)
GERD, or gastroesophageal reflux disease, is a chronic digestive condition where stomach acid flows back into the esophagus, leading to symptoms like heartburn, regurgitation, and chest discomfort, especially at night. While GERD is primarily associated with digestive symptoms, it can also disrupt sleep and indirectly contribute to night sweats.
When acid reflux occurs during sleep, the resulting discomfort or pain can trigger the body’s stress response, elevating heart rate and body temperature. In some individuals, this physiological reaction can manifest as sweating during the night, particularly if GERD episodes are frequent or severe.
Sleeping flat or on your back can make symptoms worse, while lifestyle changes—like elevating the head of the bed, avoiding late meals, and limiting trigger foods—can help manage GERD and related sleep disturbances.
Alcohol or Substance Use
Alcohol and certain recreational or prescription drugs can interfere with the body’s ability to regulate temperature during sleep. Alcohol is a vasodilator, meaning it expands blood vessels and can make you feel warm initially. However, as your body processes it, it can cause sweating, dehydration, and disrupted sleep cycles, all of which increase the likelihood of night sweats.
Similarly, withdrawal from nicotine, caffeine, or opioids can trigger night sweats as your nervous system adjusts. Stimulants like cocaine or amphetamines may also lead to elevated heart rate and body temperature during the night. If you frequently wake up sweating and use alcohol or other substances regularly, it’s worth considering how these may be impacting your sleep and whether reducing or eliminating them might help.
Neurological Conditions
Conditions that damage the brain can cause unusual and excessive sweating, including night sweats. For example, people who have had a stroke may experience excessive sweating on only one side of their body. Other neurological conditions that may cause night sweats include neuropathy, autonomic dysreflexia, and syringomyelia.
Certain Cancers
Both cancer and cancer treatments are known to cause night sweats . The symptom may occur early, mid-treatment, or even in cancer survivors whose disease is in remission. While it’s most important to treat the cancer itself, medication and lifestyle changes can reduce night sweats during and after treatment.
Lifestyle Habits
Certain daily habits can unintentionally raise your core body temperature and make it harder to stay cool during sleep. Eating spicy foods or drinking hot beverages before bed can stimulate the nervous system and increase internal heat, often leading to sweating during the night. Ingredients like capsaicin in spicy foods or the warmth of a hot drink can disrupt the body’s thermoregulation process.
Likewise, exercising too close to bedtime can have a similar effect. Physical activity elevates your body temperature and releases stimulating hormones like adrenaline, which can interfere with your ability to wind down and stay cool while you sleep.
To minimize these effects, it’s best to finish intense workouts and avoid spicy meals or hot drinks at least two to three hours before going to bed. Small changes in evening routines may help reduce the likelihood of experiencing night sweats.
How to Stop Night Sweats
Although many health conditions may cause night sweats, treating the condition often relieves the symptom. However, not all night sweats are caused by an underlying condition, and the results of treatments are not always immediate.
Home Remedies for Night Sweats
In addition to any medical treatments suggested by your doctor, other ways of relieving night sweats include:
- Breathable Bedding: Bedding and pajamas made of breathable, moisture-wicking fabric can help keep you cooler and more comfortable at night. If you regularly sweat through your bedding or clothes, consider keeping extra sets within easy reach.
- Air Conditioning: Keeping your room at a cool temperature may be more comfortable. It is also easier to sleep better when the room is not too hot, even for people who do not experience night sweats.
- Stress-Relieving Techniques: Night sweats can be stressful, as are many of the conditions that cause them. Stress also worsens night sweats, making relaxation techniques a useful approach. Some popular methods to reduce stress include mindfulness, guided imagery, meditation, and breathing exercises. Hypnosis and cognitive behavioral therapy can also help.
- Maintaining a Healthy Weight: Excess weight can be both a cause of night sweats and a risk factor for conditions that cause night sweats, such as sleep apnea.
- Avoiding Caffeine, Alcohol, and Spicy Food: These foods can affect your internal temperature and cause you to sweat. If you experience night sweats, avoiding eating or drinking these close to your bedtime may help relieve your symptoms or avoid triggering them further.
Medications for Night Sweats
When night sweats are frequent, intense, or linked to an underlying condition, medications may be recommended to help manage symptoms. The choice of medication often depends on the root cause, such as hormonal changes, mental health conditions, or chronic illness.
- Hormone therapy (HT): For women experiencing menopausal night sweats, estrogen therapy—sometimes combined with progesterone—can be effective in reducing hot flashes and nighttime sweating.
- Antidepressants: Certain low-dose antidepressants, including SSRIs and SNRIs, may help manage hot flashes and night sweats, even in women who aren’t depressed.
- Gabapentin and clonidine: These medications are sometimes prescribed off-label to reduce night sweats, especially in menopausal women or those with conditions that affect thermoregulation.
- Medications to treat the underlying cause: If night sweats are due to conditions like infections, cancer, or thyroid disease, treating the root issue with appropriate medication (like antibiotics or antithyroid drugs) can resolve the sweating.
It’s important to consult a healthcare provider to determine whether medications are appropriate, and if so, which ones are best suited to your specific symptoms and health history.
If you don’t have a doctor, Midi Health is a virtual care clinic focused on women navigating perimenopause and menopause. Along with helping you navigate sleep issues, Midi’s trained clinicians provide patients with personalized care for hot flashes and night sweats, moodiness, anxiety, brain fog, weight gain, and many more symptoms of hormonal change. Treatments may include hormonal and non-hormonal medications, supplements, and lifestyle coaching and Midi’s care is guided by world-class experts in women’s midlife health.
When to Talk to Your Doctor
Night sweats can be uncomfortable and sometimes frightening. Not all night sweats are caused by an underlying condition, but you should speak to your doctor about new or unusual night sweats, or night sweats that occur regularly and do not respond to lifestyle changes. Your doctor can take steps to diagnose any underlying health condition and ensure you receive appropriate treatment.
Other symptoms that merit a visit to your doctor if they occur with night sweats include:
- Weight loss without changing your diet or exercising more
- Unexplained fever
- Excessive daytime sleepiness and fatigue
- Muscle weakness
- Sleep disturbances
- Mood changes

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
22 Sources
-
Bryce C. (2020). Persistent night sweats: Diagnostic evaluation. American Family Physician, 102(7), 427–433.
https://pubmed.ncbi.nlm.nih.gov/32996756/ -
Kingma B, Frijns A, van Marken Lichtenbelt W. The thermoneutral zone: implications for metabolic studies. Front Biosci (Elite Ed). 2012;4(5):1975-1985. Published 2012 Jan 1. doi:10.2741/e518
https://pubmed.ncbi.nlm.nih.gov/22202013/ -
Deecher, D. C., & Dorries, K. (2007). Understanding the pathophysiology of vasomotor symptoms (hot flushes and night sweats) that occur in perimenopause, menopause, and postmenopause life stages. Archives of Women’s Mental Health, 10(6), 247–257.
https://pubmed.ncbi.nlm.nih.gov/18074100/ -
Whiteley, J., DiBonaventura, M. daCosta, Wagner, J.-S., Alvir, J., & Shah, S. (2013). The impact of menopausal symptoms on quality of life, productivity, and economic outcomes. Journal of Women’s Health (2002), 22(11), 983–990.
https://pubmed.ncbi.nlm.nih.gov/24083674/ -
Hantsoo, L., & Epperson, C. N. (2015). Premenstrual dysphoric disorder: Epidemiology and treatment. Current Psychiatry Reports, 17(11), 87.
https://pubmed.ncbi.nlm.nih.gov/26377947/ -
Thurston, R. C., Luther, J. F., Wisniewski, S. R., Eng, H., & Wisner, K. L. (2013). Prospective evaluation of nighttime hot flashes during pregnancy and postpartum. Fertility and Sterility, 100(6), 1667–1672.
https://pubmed.ncbi.nlm.nih.gov/24035604/ -
Torrealday, S., Kodaman, P., & Pal, L. (2017). Premature ovarian insufficiency—An update on recent advances in understanding and management. F1000Research, 6, 2069.
https://pubmed.ncbi.nlm.nih.gov/29225794/ -
A.D.A.M. Medical Encyclopedia. (2021, June 14). Primary ovarian insufficiency. MedlinePlus.
https://medlineplus.gov/primaryovarianinsufficiency.html -
McLean, C. P., Asnaani, A., Litz, B. T., & Hofmann, S. G. (2011). Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research, 45(8), 1027–1035.
https://pubmed.ncbi.nlm.nih.gov/21439576/ -
Wiegner, L., Hange, D., Björkelund, C., & Ahlborg, G. (2015). Prevalence of perceived stress and associations to symptoms of exhaustion, depression and anxiety in a working age population seeking primary care—An observational study. BMC Family Practice, 16, 38.
https://pubmed.ncbi.nlm.nih.gov/25880219/ -
Das, S. (2020, June). Hyperhidrosis.
https://www.merckmanuals.com/professional/dermatologic-disorders/sweating-disorders/hyperhidrosis#v963302 -
Arnardottir, E. S., Janson, C., Bjornsdottir, E., Benediktsdottir, B., Juliusson, S., Kuna, S. T., Pack, A. I., & Gislason, T. (2013). Nocturnal sweating–A common symptom of obstructive sleep apnoea: The Icelandic sleep apnoea cohort. BMJ Open, 3(5), e002795.
https://pubmed.ncbi.nlm.nih.gov/23674447/ -
Sari, R., Bayindir, Y., Sevinc, A., Bahceci, F., & Ozen, S. (2002). The triad of weight loss, fever and night sweating: Isolated bone marrow tuberculosis, a case report. Journal of Chemotherapy (Florence, Italy), 14(4), 420–422.
https://pubmed.ncbi.nlm.nih.gov/12420863/ -
Johnson, M. O., Stallworth, T., & Neilands, T. B. (2003). The drugs or the disease? Causal attributions of symptoms held by HIV-positive adults on HAART. AIDS and Behavior, 7(2), 109–117.
https://pubmed.ncbi.nlm.nih.gov/14586196/ -
Ewals, J. A. P. M. (2005). Brucellosis as an imported disease in a young man with arthritis. Nederlands Tijdschrift Voor Geneeskunde, 149(50), 2810–2814.
https://pubmed.ncbi.nlm.nih.gov/16385835/ -
Shetty, A., Ribeiro, D., Evans, A., & Linnane, S. (2004). Gonococcal endocarditis: A rare complication of a common disease. Journal of Clinical Pathology, 57(7), 780–781.
https://pubmed.ncbi.nlm.nih.gov/15220379/ -
Smetana, G. (2024 January). Evaluation of the patient with night sweats or generalized hyperhidrosis. In M. Aronson & J. Givens (Ed.). UpToDate.
https://www.uptodate.com/contents/evaluation-of-the-patient-with-night-sweats-or-generalized-hyperhidrosis -
Bryce, C. (2020). Persistent night sweats: Diagnostic evaluation. American Family Physician, 102(7), 427–433.
https://pubmed.ncbi.nlm.nih.gov/32996756/ -
Flores, S., Davis, M. D. P., Pittelkow, M. R., Sandroni, P., Weaver, A. L., & Fealey, R. D. (2015). Abnormal sweating patterns associated with itching, burning and tingling of the skin indicate possible underlying small-fibre neuropathy. The British Journal of Dermatology, 172(2), 412–418.
https://pubmed.ncbi.nlm.nih.gov/25597261/ -
Khanna, K., Theologis, A. A., & Tay, B. (2017). Autonomic dysreflexia caused by cervical stenosis. Spinal Cord Series and Cases, 3, 17102.
https://pubmed.ncbi.nlm.nih.gov/29423305/ -
Stanworth, P. A. (1982). The significance of hyperhidrosis in patients with post-traumatic syringomyelia. Paraplegia, 20(5), 282–287.
https://pubmed.ncbi.nlm.nih.gov/7177694/ -
National Cancer Institute. Hot flashes and night sweats (PDQ) – Patient version.
https://www.cancer.gov/about-cancer/treatment/side-effects/hot-flashes-pdq






