Paradoxical Sleep
As you learn about what happens when you sleep, it is common to discover seemingly contradictory pieces of information. For example, taking regular naps has been found to improve memory and learning , while also being linked to cognitive decline. While these effects seem to be at odds, this is an example of a paradox. A paradox is a set of ideas that are accurate, but appear contradictory or defy logic and common sense.
The use of the word paradoxical is widespread in sleep medicine, perhaps because sleep is a complex and often contradictory process. Some sleep concepts that include the term paradox are paradoxical sleep, paradoxical insomnia, and paradoxical intention. These three concepts describe different aspects of sleep and are not directly related to each other, but each can help you deepen your understanding of sleep health.
What Is Paradoxical Sleep?
Paradoxical sleep is one of the many names given to rapid eye movement (REM) sleep. To understand the paradox of REM sleep, it is important to know that sleep is categorized into four sleep stages, each associated with certain patterns of brain waves, eye movements, and muscle tension. The first three stages are called non-REM (NREM) sleep, and the fourth stage is called REM sleep. Most people complete four to six cycles of all the sleep stages each night.
Adults spend the majority of the night, approximately 75% to 80% of total sleep time , in non-REM sleep. During these three stages of sleep, brain waves, breathing, and heartbeat progressively slow down . In the deepest stage of non-REM sleep, muscles are relaxed and eye movements virtually stop.
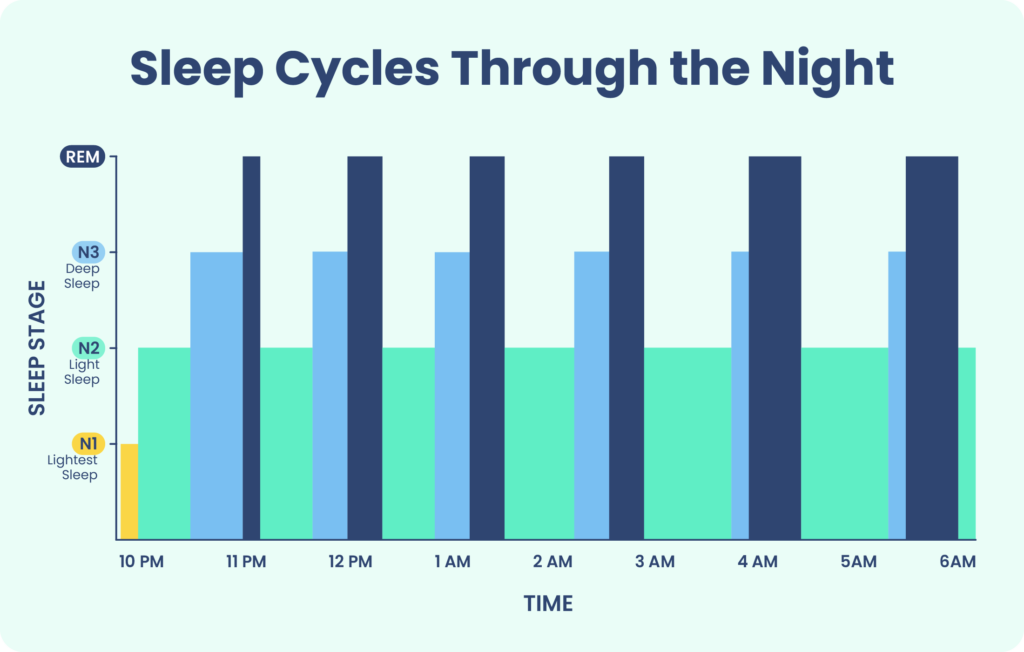
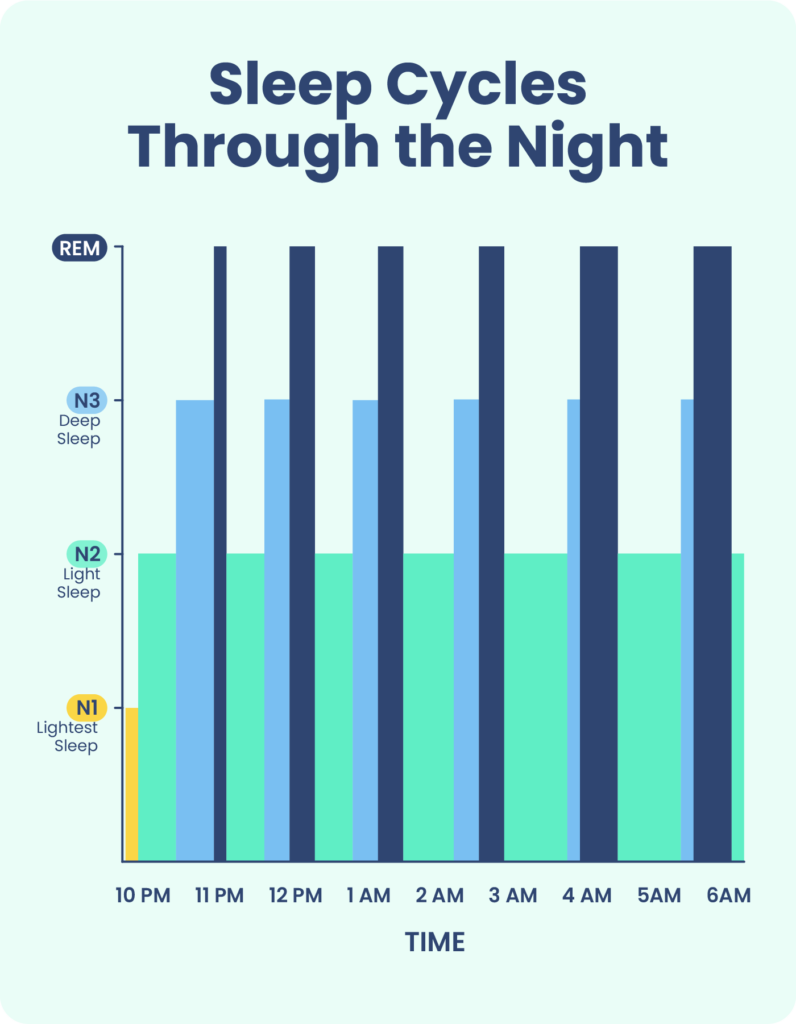
The first cycle of REM sleep begins around 60 to 90 minutes after falling asleep. In REM sleep, brain activity increases to levels similar to those seen during waking hours. At the same time, most muscles enter a state of atonia, which means that they are temporarily paralyzed. Researchers suggest that REM atonia helps to prevent sleepers from acting out their dreams.
While the purpose of REM sleep is still under debate, this sleep stage is associated with a variety of important functions including learning, memory consolidation, and creativity . REM sleep is also when most vivid dreams occur. Researchers believe that this is because a part of the brain called the thalamus becomes active during REM sleep. The thalamus processes sensory information during wake periods and shuts down during NREM sleep stages. However, it becomes active again during REM sleep and contributes to the rich sensory experiences that occur while dreaming.
Why Is REM Sleep Called Paradoxical Sleep?
Rapid eye movement (REM) sleep is called paradoxical sleep because it involves seemingly contradictory states of an active mind and a sleeping body. The term paradoxical sleep was coined by the French researcher Dr. Michel Jouvet in the late 1950s.
While investigating sleep in cats, Dr. Jouvet was the first researcher to identify the role of the brainstem in sending signals to initiate muscle atonia during REM sleep. Dr. Jouvet observed that lesions on the brainstem caused cats to lose muscle atonia, after which they appeared to act out their dreams.
Muscle atonia is affected in several sleep disorders called REM parasomnias, which involve abnormal behaviors during REM sleep . In REM sleep behavior disorder, normal muscle paralysis does not occur during REM sleep. People with this sleep disorder may act out their dreams, sometimes violently.
In another type of REM parasomnia, called sleep paralysis, muscle atonia occurs when a person is beginning to fall asleep or right as they are waking up. As features of REM sleep encroach into wakefulness during an experience of sleep paralysis, a person may have hallucinations and be fully aware of the inability to move their arms, legs, or head. Sleep paralysis usually only lasts a few minutes at most.
Paradoxical Sleep Deprivation
Paradoxical sleep deprivation is another way of saying REM sleep deprivation . Over the long term, paradoxical sleep deprivation may increase the likelihood of chronic conditions such as stress disorders and obesity . A loss of REM sleep can also happen in people with high stress levels or certain sleep disorders, such as insomnia and obstructive sleep apnea (OSA).
When you do not get enough REM sleep, the body tries to correct the deficit through REM rebound. During REM rebound, an individual catches up on missed REM sleep by experiencing a higher intensity and more frequent bouts of REM sleep. Generally, deep sleep is the first sleep stage to rebound, and REM rebound does not occur until a person is moderately to severely sleep deprived.
While many of the factors that impact the length and quality of REM sleep are out of your control, there are things you can do to protect this sleep stage. Alcohol , illicit drugs, and medications including certain antidepressants, antipsychotics, and sedatives can affect REM sleep. It is important to speak with your doctor if you have concerns about your current medications and how they may affect your sleep.
There are still many unanswered questions about what happens to your body when you lose REM sleep. Although scientists are still learning about consequences of REM sleep deprivation, it is clear that sleep deprivation in general can lead to a higher risk of weight gain, cardiovascular disease, and other health issues.
What Is Paradoxical Insomnia?
Paradoxical insomnia is a type of insomnia in which a person appears to be sleeping well based on objective measures, but they do not perceive their sleep to be restful. Although people who have this condition may sleep through the night, they often wake up feeling unrefreshed, underestimate how long they have slept, and believe they were awake during periods when they were asleep. Also called sleep state misperception, paradoxical insomnia can be a frustrating and confusing experience.
The International Classification of Sleep Disorders, Third Edition no longer divides insomnia into different subtypes, but many experts continue to find the term useful.
How Can I Tell if I Have Paradoxical Insomnia?
Since not being able to tell how long you have slept is the primary sign of this condition, it may be challenging to know if you are experiencing paradoxical insomnia. If you suspect that you may have this disorder, it is best to talk to a doctor or sleep specialist who has access to additional tools, like a sleep study.
A sleep study, or polysomnogram, can measure brain waves and other data while you sleep. These data may show that a person with paradoxical insomnia is getting more sleep than they report. While this means that a sleep study could theoretically diagnose this condition, unfortunately paradoxical insomnia is difficult to diagnose.
Researchers have not been able to pinpoint markers of sleep state misperception based on brain waves, sleep diaries, or tools that measure sleep versus wake based on body movements, and experts are divided on whether paradoxical insomnia should be considered a distinct disorder.
Paradoxical Intention as a Treatment for Insomnia
Paradoxical intention is a simple technique designed to facilitate falling asleep. The idea behind this technique is that people with insomnia develop anxiety that increases the more they try to fall asleep .
To decrease the anxiety of trying to fall asleep, paradoxical intention instructs sleepers to take a counterintuitive approach and try to stay awake in bed for as long as they can. Ideally, removing the pressure to fall asleep should paradoxically make it easier to doze off. In one study, adults who used paradoxical intention fell asleep almost half an hour faster than those who did not. However, more high-quality studies are needed to confirm whether this method is effective.
One drawback of paradoxical intention is that it is difficult to persuade people to try this technique, as the premise may increase anxiety in people who already experience stress at bedtime.
When to Talk to Your Doctor
Whether you are concerned about getting enough REM sleep or thinking about trying paradoxical intention to manage insomnia, working with a doctor or sleep specialist can help. A doctor can address any questions or concerns you have, order tests if necessary, and assist you in developing a strategy for improving the length and quality of your sleep.
References
19 Sources
-
Mantua, J., & Spencer, R. (2017). Exploring the nap paradox: Are mid-day sleep bouts a friend or foe? Sleep Medicine, 37, 88–97.
https://pubmed.ncbi.nlm.nih.gov/28899546/ -
Blumberg, M. S., Lesku, J. A., Libourel, P. A., Schmidt, M. H., & Rattenborg, N. C. (2020). What is REM sleep?. Current Biology, 30(1), R38–R49.
https://pubmed.ncbi.nlm.nih.gov/31910377/ -
Patel, A. K., Reddy V., Araujo J. F. (2019, March). Physiology, sleep stages. StatPearls., Retrieved February 17, 2022, from
https://pubmed.ncbi.nlm.nih.gov/30252388/ -
Schwab, R. J. (2020, June). Overview of sleep. Merck Manual Consumer Version., Retrieved February 17, 2022, from
https://www.merckmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/overview-of-sleep -
National Institute of Neurological Disorders and Strokes (NINDS). (2019, August 13). Brain basics: Understanding Sleep., Retrieved February 17, 2022, from
https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep -
Feriante, J., & Araujo, J. F. (2021, February). Physiology, REM sleep. StatPearls., Retrieved February 17, 2022, from
https://www.ncbi.nlm.nih.gov/books/NBK531454/ -
Peever, J., & Fuller, P. M. (2017). The biology of REM sleep. Current Biology, 27(22), R1237-R1248.
https://pubmed.ncbi.nlm.nih.gov/29161567/ -
Lewis, P. A., Knoblich, G., & Poe, G. (2018). How memory replay in sleep boosts creative problem-solving. Trends in Cognitive Sciences, 22(6), 491–503.
https://pubmed.ncbi.nlm.nih.gov/29776467/ -
Siegel, J. M. (2011). REM sleep: A biological and psychological paradox. Sleep Medicine Reviews, 15(3), 139–142.
https://pubmed.ncbi.nlm.nih.gov/21482156/ -
Luppi P., H. (2018). Jouvet’s animal model of RBD, clinical RBD, and their relationships to REM sleep mechanisms. Sleep Medicine, 49, 28–30.
https://pubmed.ncbi.nlm.nih.gov/30172630/ -
American Academy of Sleep Medicine. (2014). The International Classification of Sleep Disorders – Third Edition (ICSD-3). Darien, IL.
https://aasm.org/ -
Tufik, S., Andersen, M. L., Bittencourt, L. R., & Mello, M. T. (2009). Paradoxical sleep deprivation: Neurochemical, hormonal and behavioral alterations. Evidence from 30 years of research. Anais da Academia Brasileira de Ciencias, 81(3), 521–538.
https://pubmed.ncbi.nlm.nih.gov/19722021/ -
Feriante J, Singh S. (2020, July 19). REM Rebound Effect. StatPearls Publishing., Retrieved February 17, 2022, from
https://www.ncbi.nlm.nih.gov/books/NBK560713/ -
Colrain, I. M., Nicholas, C. L., & Baker, F. C. (2014). Alcohol and the sleeping brain. Handbook of Clinical Neurology, 125, 415–431.
https://pubmed.ncbi.nlm.nih.gov/25307588/ -
Afkhamnejad, E., Kumar, S. (2018). The role of prescription drugs in REM sleep. Neurology, 90(15).
https://n.neurology.org/content/90/15_Supplement/P1.109 -
Watson, C. J., Baghdoyan, H. A., & Lydic, R. (2010). Neuropharmacology of sleep and wakefulness. Sleep Medicine Clinics, 5(4), 513–528.
https://pubmed.ncbi.nlm.nih.gov/21278831/ -
Rezaie, L., Fobian, A. D., McCall, W. V., & Khazaie, H. (2018). Paradoxical insomnia and subjective-objective sleep discrepancy: A review. Sleep Medicine Reviews, 40, 196–202.
https://pubmed.ncbi.nlm.nih.gov/29402512/ -
Holley A. B. (2016). Perceiving the misperception. Journal of Clinical Sleep Medicine, 12(9), 1211–1212.
https://pubmed.ncbi.nlm.nih.gov/27568905/ -
Edinger, J. D., Arnedt, J. T., Bertisch, S. M., Carney, C. E., Harrington, J. J., Lichstein, K. L., Sateia, M. J., Troxel, W. M., Zhou, E. S., Kazmi, U., Heald, J. L., & Martin, J. L. (2021). Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine, 17(2), 263–298.
https://pubmed.ncbi.nlm.nih.gov/33164741/